Evaluation of surgeon-performed ultrasound usage amongst Australian and New Zealand Endocrine Surgeons
Introduction
Over the past two decades, surgeons in multiple subspecialties have increasingly adopted ultrasound (US) as a diagnostic and interventional tool in both office and operating theatre environments (1-3). Technological advances in US have led to the development of small and portable devices, which can produce high resolution images comparable to high-end radiological US units. Many of these devices are now available in a tablet, mobile phone or a laptop.
US is recognized as the gold standard for the assessment of the thyroid and parathyroid glands (3,4). It is also helpful for the evaluation of cervical lymph nodes (3,4). Endocrine surgeon-performed US has significant advantages for patients including reduced number of visits, less waiting time to surgery and overall cost efficiencies (5,6). US fine needle aspirate biopsy (FNAB) performed by endocrine surgeons have been shown to be comparable to interventions performed by radiologists, in their sensitivity, specificity, non-diagnostic, and complication rates (7,8).
Whilst it has been appreciated anecdotally that endocrine surgeons are increasingly embracing the use of US, the true extent of the adoption of US by endocrine surgeons in Australia and New Zealand has not been previously documented. The purpose of this study was to evaluate the patterns of US utilization amongst Australian and New Zealand Endocrine Surgeon (ANZES) member endocrine surgeons by means of an online survey. We present the following article in accordance with the SURGE reporting checklist (available at https://aot.amegroups.com/article/view/10.21037/aot-22-8/rc).
Methods
Registered members (consultants) of the ANZES were invited to participate in an online survey of their personal usage and application of endocrine US within their clinical practices. Survey was created using the platform Qualtrics XM© and the survey included 15 multichoice questions (Table 1). The questions were subdivided into four main sections, including demographic information, access to US, patterns of US usage, and US training and accreditation.
Table 1
| Query |
|---|
| Demographics |
| 1. Which of the following best describes the predominant nature of your practice? |
| a. Endocrine Surgery exclusively |
| b. Breast and Endocrine Surgery |
| c. Breast and Endocrine Surgery, some General Surgery |
| d. General Surgery with an Endocrine Surgery Interest |
| e. General Surgery with an Endocrine and Breast Surgery Interest |
| 2. Where is your main practice base? |
| a. Metropolitan |
| b. Regional/Rural |
| 3. Which of the following best describes your practice? |
| a. Private Practice Only |
| b. Public Practice Only |
| c. Both Private and Public Practice |
| 4. How many years have you been practising as a Specialist Endocrine Surgeon? |
| Access to ultrasound |
| 5. Do you believe there is a role for surgeon-performed US in an endocrine surgical practice? |
| a. Not necessary |
| b. Helpful, but a luxury |
| c. Important and very desirable |
| d. Essential for best practice |
| 6. How would you describe your access to a portable US machine? |
| a. I have full-time access to a portable US machine |
| b. I share a portable US machine in a group practice |
| c. I do not have ready access to a portable US machine, and do not personally use US |
| Ultrasound utilization |
| 7. How many Surgeon-performed ultrasounds would you perform per month? |
| a. None |
| b. 1–10 |
| c. 11–20 |
| d. >20 |
| 8. Do you perform needle biopsies under ultrasound in your practice? |
| a. I do not perform office-based biopsies |
| b. I perform FNAB under US guidance |
| 9. How many Surgeon-performed ultrasound-guided FNA biopsies do you perform at your practice per month? |
| a. None |
| b. 1–5 |
| c. 6–10 |
| d. >10 |
| 10. When undertaking parathyroid, thyroid, or cervical lymph node resections, do you utilize ultrasound in the OR? (multiple answers allowed) |
| a. I use US to plan, map out or assist with parathyroid surgery in the OR |
| b. I use US to plan, map out or assist with thyroid surgery in the OR |
| c. I use US to plan, map out or assist with cervical lymph node resections in the OR |
| d. I DO NOT use US in endocrine surgical procedures |
| Ultrasound training and accreditation |
| 11. I have been using US in my practice for |
| a. Less than 1 year |
| b. 1 to 3 years |
| c. Over 3 years |
| d. I do not use US |
| 12. Have you fulfilled the Department of Health & Ageing Diagnostic Imaging Accreditation Scheme requirements to be eligible for Medicare funding of US services? |
| a. Yes |
| b. No |
| 13. Have you achieved accreditation for the ASUM Endocrine CCPU? |
| a. Yes |
| b. No |
| 14. Which of the following best describes your training in Endocrine US? |
| a. I have received US training as part of my SET/Registrar FRACS training |
| b. I have received formal training post-Fellowship through structured courses/workshops |
| c. I have received no formal training in US, self-taught |
| d. I do not use US in my practice |
| 15. For Endocrine Surgeons to be adequately trained in Surgeon-performed ultrasound techniques, which of those listed below do you feel is the most appropriate forum for this training to be conducted? (multiple answers allowed) |
| a. During FRACS SET/Registrar training |
| b. PFTP i.e., While serving in a Fellow position |
| c. Structured training programmes (e.g., ASUM Endocrine CCPU) |
| d. Informal training by Mentors |
US, ultrasound; FNAB, fine needle aspirate biopsy; FNA, fine needle aspirate; OR, operating room; ASUM, Australasian Society for Ultrasound in Medicine; CCPU, Certificate in Clinician Performed Ultrasound; SET, surgical education and training; FRACS, Fellow of the Royal Australasian College of Surgeons; PFTP, post fellowship training.
The link to the voluntary survey was disseminated electronically twice to all members of ANZES between August and September 2021. Participants’ informed consents were requested. To ensure privacy of the participants, responses were anonymous, and details were not disclosed. This research is of negligible risk and as such a formal ethical approval was not required. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). To ensure that each member only completed one survey, the respondent’s IP address was recorded upon submission of a completed survey.
Statistical analysis
Continuous variables were summarized as median and range and categorical variables as frequencies and percentages. Chi-squared analysis and Fischer’s exact test were used where appropriate for comparisons of data. All statistical analyses were performed using Statistical Package for Social Sciences (SPSS). P values <0.05 were deemed significant.
Results
Following the invitation to participate in the survey on two separate occasions, one month apart, 52 of 125 (42%) invited endocrine surgeons responded to the survey. There was no missing data.
Practice demographics
Among the respondents, only 11 (21%) practiced endocrine surgery exclusively, 16 (31%) practiced both breast and endocrine surgery, and the remaining 25 (48%) had practices that were a mixture of breast, endocrine and general surgery (Figure 1). The majority of the respondents, 47 (90%), had practices located in a metropolitan precinct, with only 5 (10%) located in regional or rural settings (Table 2). Most surgeons, 42 (81%), worked in both and private and public sectors, with 13% in private practice and 6% in public practice only. Of the respondents, the median number of years practicing as a surgeon was 13 years (range, 1–35 years).
Table 2
| Surgical practice | Value (N=52), n (%) |
|---|---|
| Practice specialties | |
| Endocrine surgery exclusively | 11 [21] |
| Breast and endocrine surgery | 16 [31] |
| Breast and endocrine surgery, some general surgery | 20 [38] |
| General surgery with an endocrine surgery interest | 2 [4] |
| General surgery with an endocrine and breast surgery interest | 3 [6] |
| Practice location | |
| Metropolitan | 47 [90] |
| Regional/rural | 5 [10] |
| Nature of practice | |
| Private practice only | 7 [13] |
| Public practice only | 3 [6] |
| Both private and public practice | 42 [81] |
| Years of practice as surgeon | 13 (range, 1–35) |
Access to US
Most surgeons, 38 (73%), had fulltime access to a portable US machine, whilst 4 (8%) had shared access, and with 10 (19%) having no access to an US device. There was no statistically significant difference in access to US for surgeons who practice endocrine exclusively versus those who do not (P=1.00).
Patterns of US utilization
Forty-two (80%) surgeons responded that surgeon-performed US in endocrine surgery practice was either important and very desirable or essential for best practice. Of the 10 respondents who felt that surgeon performed US was either not necessary or simply a luxury, 7 had no access to US equipment and 1 had only shared access. Conversely, of the 42 surgeons who had full time or shared access to US, only 3 (7.1%) considered surgeon performed US to be unnecessary or merely a luxury.
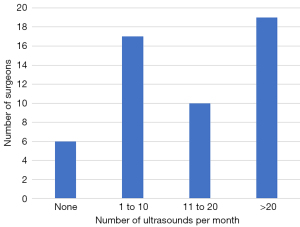
There was no statistically significant difference in access to US for surgeons who practice endocrine exclusively versus those who do not (P=0.37). Thirty-three percent of surgeons performed 1–10 US per month, 19% performed 11–20 US per month and 37% performed more than 20 US per month (Figure 2).
Only 40% (n=21) of respondents undertake US-guided FNAB however of those that do, 19% performed 1–5 FNAB’s per month, 6% performed 6–10 FNAB’s per month and 17% performed more than 10 FNAB’s per month (Figure 3). There was no statistically significant difference in US FNAB performed in metropolitan versus regional/rural settings (P=0.64).
Surgeons were questioned as to the usage of US in the operating room in the context of undertaking parathyroid, thyroid, or cervical lymph node surgery. Interestingly, 38 (73%) of Surgeons reported using US to plan, map out or assist with parathyroid surgery, 20 (38%) with thyroid surgery and 23 (44%) using US to assist with the resection of cervical lymph nodes in the operating theatre (Table 3).
Table 3
| US utilization | Value (N=52), n (%) |
|---|---|
| Role of surgeon performed US in endocrine surgical practice | |
| Not necessary | 2 [4] |
| Helpful, but a luxury | 8 [15] |
| Important and very desirable | 20 [38] |
| Essential for best practice | 22 [42] |
| Access to portable US machine | |
| Full-time access | 38 [73] |
| Sharing US machine | 4 [8] |
| No access | 10 [19] |
| Number of Surgeon-performed US per month | |
| None | 6 [12] |
| 1–10 | 17 [33] |
| 11–20 | 10 [19] |
| >20 | 19 [37] |
| US-guided needle biopsies | |
| Do not perform office-based biopsies | 31 [60] |
| FNAB under US guidance | 21 [40] |
| Number of Surgeon performed US-guided FNA biopsies per month | |
| None | 30 [58] |
| 1–5 | 10 [19] |
| 6–10 | 3 [6] |
| >10 | 9 [17] |
| US usage in operating theatre | |
| Parathyroid surgery | 38 [73] |
| Thyroid surgery | 20 [38] |
| Cervical lymph node surgery | 23 [44] |
| Do not use US | 10 [19] |
US, ultrasound; FNAB, fine needle aspirate biopsy; FNA, fine needle aspirate.
Experience and attitudes to US training
Seventy-nine percent of surgeons had been performing US for more than 3 years. The Department of Health and Ageing conduct a Diagnostic Imaging Assessment Scheme (DIAS) to determine eligibility for Medicare funding for US services (9). Interestingly, 29 (56%) of respondents had successfully completed those requirements. However, only 20 (38%) surgeons had achieved accreditation with a Certificate in Clinical Performed Ultrasound (CCPU) conducted by the Australian Society of Ultrasound in Medicine (ASUM).
Most respondents 42 (81%) indicated their training in US had been achieved post fellowship through formal training courses, whereas only 4% of surgeons had received US teaching as a surgical education and training (SET) trainee/registrar.
When questioned as to what they believed to be the best format for US training (multiple answers allowed), respondents affirmed all avenues for US training to be desirable, with post fellowship training achieving the highest score (88%), followed by structured training programs compliant with the ASUM CCPU (63%). Forty-four percent of surgeons indicated that training should commence as a SET trainee/Registrar, and 31% advocated informal training by mentors (Table 4).
Table 4
| US training and accreditation | Value (N=52), n (%) |
|---|---|
| Duration of US usage | |
| Less than 1 year | 1 [2] |
| 1 to 3 years | 4 [8] |
| Over 3 years | 41 [79] |
| I do not use US | 6 [12] |
| Completed diagnostic imaging accreditation scheme requirements | |
| Yes | 29 [56] |
| No | 23 [44] |
| ASUM CCPU accreditation | |
| Yes | 20 [38] |
| No | 32 [62] |
| Endocrine US training | |
| SET/registrar FRACS training | 2 [4] |
| Formal training post-fellowship | 42 [81] |
| No formal training in US, self-taught | 6 [12] |
| Do not use Ultrasound | 2 [4] |
| Preferred model of endocrine US training | |
| During FRACS SET/registrar training | 23 [44] |
| Post-Fellowship training | 46 [88] |
| Structured training programmes ASUM Endocrine CCPU | 33 [63] |
| Informal training by mentors | 16 [31] |
US, ultrasound; ASUM, Australasian Society for Ultrasound in Medicine; CCPU, Certificate in Clinician Performed Ultrasound; SET, surgical education and training; FRACS, Fellow of the Royal Australasian College of Surgeons.
Discussion
The results of this study indicate that endocrine surgeons in Australia and New Zealand have embraced usage of US in clinical practice in both the office and operating theatre, with 80% indicating that surgeon-performed US is important and desirable, or essential for best practice. There was no statistically significant difference those who practice endocrine surgery exclusively versus those who do not (P=1.00). Forty-two (81%) surgeons surveyed had fulltime access or the ability to share US equipment, and of these 39 (92.9%) considered surgeon performed US to be either important or essential for best practice. Interestingly, the majority of surgeons (56%) are performing more than 10 US examinations per month. However, only 40% of those surveyed undertake US guided FNAB, with only 17% performing more than 10 FNAB a month. Although training may be a factor, time constraint and limited resource such as the availability of a cytologist, may be other factors contributing to the lower percentage of surgeons performing fine needle aspiration (FNA). A high proportion (73%) of surgeons utilize US for parathyroid surgery, 38% for thyroid surgery and 44% to localize cervical lymph nodes for excision.
Surgeon-performed US is increasingly recognized as an important tool to provide better and more efficient outcomes for patients (5,6). Endocrine surgeons are in a unique position to develop expertise in thyroid and parathyroid US based on its use in investigation, followed by feedback obtained from subsequent surgical procedures. In addition, access to compact US devices has increased in recent years as a result of improved imaging technology. This enables high resolution images to be achieved, collected, and stored in laptops, tablets, and smart phones. At the same time, the cost of US machines has significantly decreased. This increases accessibility for medical practitioners to incorporate US into their clinical armamentarium.
Endocrine surgeons are cognizant of US features of thyroid nodules and malignancies and are familiar with the American College of Radiology Thyroid Imaging Reporting & Data System (ACR TI-RADS) (10). An international survey of 7 different otolaryngology and endocrine/general surgery associations across 52 countries including the International Association of Endocrine Surgery (IAES) showed that 33% of participants report routinely performing their own neck US (11). In another international survey, 59% of both fellowship and non-fellowship-trained endocrine surgeons currently use US in their practice (12).
US enables interval assessment of thyroid nodules and facilitates FNAB (7). Multiple studies have shown that surgeon-performed US-FNAB is safe and effective, with sensitivity, specificity, non-diagnostic, and complication rates which are comparable or superior to radiologically performed US (5,7). Endocrine surgeons are therefore well placed to utilize US in clinical setting, particularly in achieving the one-stop shop thyroid evaluation. Patel et al. demonstrated a 41% reduction of patients attending the radiology department for FNAB (5). The mean time to establish a diagnosis in surgeon-performed US-FNAB was 1 working day, compared to 29.5 working days for radiologically performed US FNAB (P<0.001) in a Singaporean study (13). Another study by Al-azawi et al. showed that patients with thyroid cancer also had a shorter time to surgery in the surgeon-performed US group (mean 15.3 days) compared to the radiologist’ group (mean 53.3 days, P=0.01) (7). A New Zealand study by Reeves et al. also demonstrated a reduction of time from first appointment to definitive management (47 days in surgeon-performed US- FNAB group vs. 116 days in radiology group, P<0.001) and the average costs of surgeon-performed US-FNAB was almost 40% less than a radiological US-FNAB (6).
Surgeon-performed US has improved diagnosis and altered management of patients (7,8,14). In one study, 20% of patients were noted to have suspicious thyroid nodules which warranted FNAB, 29% with suspicious lymphadenopathy and 6.1% with parathyroid adenoma, all of which were missed in the initial US (8). However, it is important to appreciate that endocrine surgeon-performed sonography is mainly practiced in the context of point-of-care US, whereby endocrine surgeons are predominantly using US to manage and treat already identified pathology. In this circumstance, endocrine surgeons are not intending to compete with their radiologist colleagues in the field of sonography, but instead are acting in a complementary fashion with the aim of streamlining patient care.
Formal training and teaching in US usage are critical not only to the maintenance of standards, but also forms the basis of appropriate credentialling. In Australia, US workshops for surgeons have been conducted through the Royal Australian College of Surgeons, through the ANZES, and General Surgeons of Australia. ASUM accreditation in CCPU included an online physics tutorial, a structured workshop accredited by ASUM and a logbook. Structured teaching workshops have demonstrated an improvement in confidence and recognizable upskilling of participants (15,16). The results of this current study indicated that whilst 56% of participants have completed the Medicare Diagnostic Imaging Accreditation Scheme (DIAS) credentialing, which is required for purposes of achieving Medicare remuneration, only 38% of respondents had achieved the ASUM CCPU accreditation.
The responses from participants in relation to preferred models of endocrine US training suggest that endocrine surgeons would be keen to see US teaching in as many forums as possible, including post-Fellowship training (88%), structured training programs approved by ASUM (63%) and SET registrar training (44%), as well as ongoing informal training by mentors (31%). A survey of IAES and American Association of Endocrine Surgeons in 2010 reported 38% of surgeons performing US of having no formal US training of any kind (12). Of surgeons completing an endocrine surgery fellowship, 85% did not have formal US training and 31% pursued training after entering practice (12).
US is an integral part of an endocrine surgeon’s practice. There is therefore an urgent imperative formalization of US training and accreditation in the curriculum of endocrine surgical fellowship in Australia and New Zealand. Promotion of US training as a part of SET General Surgical program is also important. Endocrine surgeons utilizing US should also be encouraged to achieve formal accreditation through the ASUM CCPU program which also provides credentialing of ongoing maintenance of practice standards.
Limitation included the survey response rate (42%), which is comparable to other studies (24%) (12,16), and its restriction to fulltime members of ANZES. It could be argued that endocrine surgeons who use US are more likely to participate in the survey so that the proportion of surgeons utilizing US might be less than the impression created by the survey results. The survey was initiated at a busy time of the year, and at the time of a number of disruptions throughout several Australian states when Covid related lockdowns were in place. Several other surveys were also initiated at around the same time by ANZES, so that there may have also been an issue of survey fatigue.
Conclusions
The survey demonstrates that surgeon-performed US is being significantly embraced by endocrine surgeons and members of the ANZES, with 80% of respondents overall and 92.9% of those with access to US, indicating that surgeon-performed US is essential or at least very important for best practice. Whilst a high proportion of endocrine surgeons are utilizing US in the operating theatre, a lesser percentage of surgeons are performing US FNAB, a statistic which could be related to and improved by the development of more formal training programs. There is an important need for the development and formalization of endocrine US training courses from the SET/Registrar level through to the post-Fellowship environment.
Acknowledgments
The authors are grateful to the Australian and New Zealand Endocrine Surgeons for support in providing access to the membership mailing list and distributing the survey. This abstract was accepted for a poster presentation at the RACS Annual Scientific Congress 2022.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the SURGE reporting checklist. Available at https://aot.amegroups.com/article/view/10.21037/aot-22-8/rc
Data Sharing Statement: Available at https://aot.amegroups.com/article/view/10.21037/aot-22-8/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aot.amegroups.com/article/view/10.21037/aot-22-8/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This research is of negligible risk and as such a formal ethical approval is not required. This was a voluntary survey, where participants’ informed consents were requested. We complied with privacy restrictions in that individual surgeon’s details and responses were anonymous, and details were not disclosed. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ahn D, Kim H, Sohn JH, et al. Surgeon-performed ultrasound-guided fine-needle aspiration cytology of head and neck mass lesions: sampling adequacy and diagnostic accuracy. Ann Surg Oncol 2015;22:1360-5. [Crossref] [PubMed]
- Bennett I, Khoo JF, De Viana D, et al. Australian breast surgeons and ultrasound usage: Have practices changed? Australas J Ultrasound Med 2021;24:217-24. [Crossref] [PubMed]
- Milas M, Stephen A, Berber E, et al. Ultrasonography for the endocrine surgeon: a valuable clinical tool that enhances diagnostic and therapeutic outcomes. Surgery 2005;138:1193-200; discussion 1200-1. [Crossref] [PubMed]
- Kahramangil B, Kose E, Donmez M, et al. Efficacy of surgeon-performed, ultrasound-guided lymph node fine needle aspiration in patients with thyroid pathologic conditions. Surgery 2018;164:657-64. [Crossref] [PubMed]
- Patel R, R, Skandarajah A, Gorelik A, et al. One-stop thyroid nodule clinic with same-day fine-needle aspiration cytology improves efficiency of care. ANZ J Surg 2018;88:354-8. [Crossref] [PubMed]
- Reeves M, Patel R, Harmston C. Surgeon-performed ultrasound-guided fine needle aspiration of thyroid nodules is cost effective and efficient: evaluation of thyroid nodule assessment in a provincial New Zealand hospital. N Z Med J 2019;132:60-5. [PubMed]
- Al-azawi D, Mann GB, Judson RT, et al. Endocrine surgeon-performed US guided thyroid FNAC is accurate and efficient. World J Surg 2012;36:1947-52. [Crossref] [PubMed]
- Shalaby M, Hadedeya D, Lee GS, et al. Impact of Surgeon-Performed Ultrasound on Treatment of Thyroid Cancer Patients. Am Surg 2020;86:1148-52. [Crossref] [PubMed]
- The Department of Health and Aged Care. The Diagnostic Imaging Accreditation Scheme (DIAS) 2021. Available online: https://www1.health.gov.au/internet/main/publishing.nsf/Content/di-quality
- Tessler FN, Middleton WD, Grant EG, et al. ACR Thyroid Imaging, Reporting and Data System (TI-RADS): White Paper of the ACR TI-RADS Committee. J Am Coll Radiol 2017;14:587-95. [Crossref] [PubMed]
- Maniakas A, Christopoulos A, Bissada E, et al. Perioperative practices in thyroid surgery: An international survey. Head Neck 2017;39:1296-305. [Crossref] [PubMed]
- Miller BS, Gauger PG, Broome JT, et al. An international perspective on ultrasound training and use for thyroid and parathyroid disease. World J Surg 2010;34:1157-63. [Crossref] [PubMed]
- Gu WX, Tan CS, Ho TW. Surgeon-Performed Ultrasound-Guided Fine-Needle Aspiration Cytology (SP-US-FNAC) Shortens Time for Diagnosis of Thyroid Nodules. Ann Acad Med Singap 2014;43:320-4. [Crossref] [PubMed]
- Carneiro-Pla D, Amin S. Comparison between preconsultation ultrasonography and office surgeon-performed ultrasound in patients with thyroid cancer. World J Surg 2014;38:622-7. [Crossref] [PubMed]
- Law MT, Bennett IC. Structured ultrasonography workshop for breast surgeons: is it an effective training tool? World J Surg 2010;34:549-54. [Crossref] [PubMed]
- Sharma GK, Sofferman RA, Armstrong WB. Evaluation of the American college of surgeons thyroid and parathyroid ultrasound course: Results of a web-based survey. Laryngoscope 2017;127:1950-8. [Crossref] [PubMed]
Cite this article as: Wong J, Miller JA, Bennett I. Evaluation of surgeon-performed ultrasound usage amongst Australian and New Zealand Endocrine Surgeons. Ann Thyroid 2022;7:14.