A narrative review of transoral thyroidectomy—2021 update
Introduction
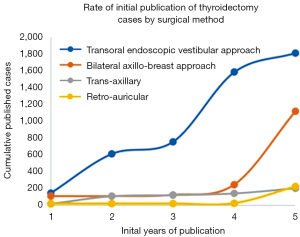
The transoral endoscopic thyroidectomy vestibular approach (TOETVA) has been increasingly studied since it was first published in 2010 by Wilhelm et al. (1,2). The technique underwent subsequent modifications in order to be performed with laparoscopic instruments, and the first clinical series followed in 2015 and 2016 by Yang et al. (3) and Anuwong (4) respectively. Since then, over 2,000 cases have been described in the literature (5). When examining the first 5 years of publication of various remote access thyroidectomy techniques, the early rates of adoption TOETVA comparatively exceeds that of trans-axillary, bilateral axillo-breast, and retro-auricular approaches (6) (Figure 1).
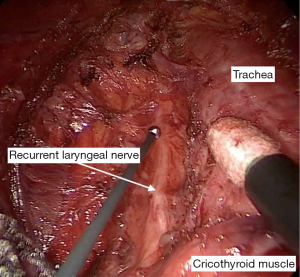
The primary advantage to TOETVA over other remote access approaches is the avoidance of a cutaneous scar. While other approaches have moved the incision to a less conspicuous location, a cutaneous scar and dissection through extended tissue planes are still required. TOETVA utilizes three mucosal incisions above the gingivobuccal sulcus which avoids a cutaneous scar, as well as provides a more direct route to the bilateral central neck and visualization of the recurrent laryngeal nerve (RLN) at its insertion (7) (Figure 2). Although there is less dissection required in TOETVA than other remote access approaches, the distance of dissection from the mentum to the central neck is greater than what would be performed in an open procedure, and therefore remote access approaches cannot truly be termed “minimally invasive” procedure.
The effect of a visible scar cannot be discounted, especially as patients and clinicians may have different perceptions of a scars’ appearance and what constitutes a cosmetically pleasing result (8). Several studies have found that scar concerns are a more common complication of thyroid surgery than RLN injury, hematoma, hypoparathyroidism, dysphagia or dysphonia (8,9). The impact of a cervical scar on quality of life is becoming more seriously examined. Despite the excellent prognosis of thyroid cancer, scar dissatisfaction has been found to be associated with decreased quality of life outcomes, poor self-perception, gaze distraction (10,11), and impaired social functioning (9,12,13). These disparities are still present even years after surgery (9).
This article will review the most recently published data on TOETVA in order to provide an update on the safety profile given the increasingly widespread performance of the procedure. We will also discuss new innovations and modifications to the technique. We wish to assess if current TOETVA complication rates and oncologic outcomes are comparable to transcervical approach (TCA) and identify areas of future research. We present the following article in accordance with the Narrative Review reporting checklist (available at https://aot.amegroups.com/article/view/10.21037/aot-22-5/rc).
Methods
A systemic literature review was conducted in order to identify the most recently published outcomes and innovations in TOETVA surgery. Utilizing PubMed, SCOPUS and Google Scholar, the terms “endoscopic transoral”, “endoscopic oral vestibular”, and “TOETVA” were combined with “thyroidectomy” or “outcomes” or “complications” to identify studies published with greater than 5 cases between January 1, 2020–February 1, 2022. Series including robotic assisted procedures were not included (Table 1).
Table 1
| Items | Specification |
|---|---|
| Date of search | February 1, 2022 |
| Databases and other sources searched | PubMed, SCOPUS, Google Scholar |
| Search terms used | “transoral” OR “endoscopic oral vestibular” OR “TOETVA” AND “thyroidectomy” OR “outcomes” OR “complications” OR “recurrence” OR “cosmesis” |
| Timeframe | 1/2020–2/2022 |
| Inclusion and exclusion criteria | Case series and meta-analyses published in the English language with at least 5 cases were included. Robotic assisted cases were excluded |
| Selection process | SAW did the article selection |
| Any additional considerations, if applicable | Additional articles recommended by JOR |
Indications
It is estimated that 55% of all patient undergoing thyroid surgery in the United States are eligible for TOETVA (14). The patient must be motivated to avoid an anterior cervical incision or have a history of keloid formation or hypertrophic scarring. Absolute size cutoffs may be institutional or surgeon specific. Published recommendations suggest a lobe no greater than 8–10 cm (4,5,7,14,15), single benign nodule no greater than 4–6 cm (3,14,16,17), and malignant nodules less than 2 cm (5,18,19). Absolute contraindications include preoperative RLN paralysis, inability to tolerate general anesthesia, lateral nodal metastases, and evidence of extrathyroidal extension into neighboring structures such as the esophagus or trachea (5,7,14,19,20). Relative contraindications include previous transoral neck surgery and radiation (5). Increased body mass index (BMI) is not a contraindication, as it does not increase the likelihood of complication (21-23), but it may make elevating skin flaps more difficult (19).
Other characteristics of the thyroid itself are critical to be considered by the surgeon before committing to a transoral approach. Conditions such as Graves’ disease or chronic Hashimoto’s may make the gland more friable (15,19,24) and increase the difficulty of the case. Tumors that are in close relationship with the course of the RLN may be more difficult to satisfactorily and safely remove utilizing a transoral approach. If there are concerns regarding the ability to obtain an appropriate and safe oncologic resection, TOETVA should be reconsidered.
Safety/complications
With the advent of any new technology, the concerns of safety and patient outcomes should remain paramount. As thyroid disease and thyroid malignancy are generally indolent with low disease-related morbidity and mortality (25), it is imperative that the treatment is not worse than the disease. The traditional TCA to thyroidectomy has low complication rates (26,27) and therefore the impetus is on TOETVA to perform at this level.
Appropriately, the safety profile of TOETVA is a focus of research. Previously published studies from multiple countries have demonstrated low complication rates comparable to TCA thyroidectomy (16,28-31). In a 2020 global review of 1,880 published TOETVA cases the rates of complications such as hematoma (0.4%), transient RLN palsy (3.9%), permanent RLN palsy (0.6%), transient hypoparathyroidism (16.8%), permanent hypoparathyroidism (0.9%) and infection (1.1%) were similar to a conventional approach and are reflective of the overall safety of this method (6). In Wang et al.’s 2021 meta-analysis of 478 TOETVA patients and 673 TCA patients (32), there was no significant difference in transient or permanent RLN palsy (OR, 1.01, P=0.98 and OR, 3.04, P=0.50), transient hypocalcemia (OR, 0.96, P=0.89), permanent hypocalcemia (OR, 0.32, P=0.49) or hematoma (OR, 7.93, P=0.05) between the two operative techniques. de Vries et al. also published a large meta-analysis in 2021 of several minimally invasive techniques including 736 TOETVA patients (33). The median incidence of a temporary RLN palsy was 4.0%, comparable to the 3.3% in the standard of care open thyroidectomy group (P=0.74).
With TOETVA being performed in countries worldwide, publication has become more prolific and there have been multiple large case series published within the last 2 years. The largest North American single-center study of 200 TOETVA cases was published in 2021 by Russell et al. (21). Their study showed no difference in the incidence of major complications between TOETVA and TCA (1.5% vs. 2.1%, P=0.75). Temporary RLN injury occurred in 4.5% vs. 2.1% (P=0.124) and temporary hypoparathyroidism in 18.2% vs 12.5% (P=0.163) of TOETVA and TCA patients respectively. Importantly, a higher BMI was not associated with a higher odds ratio of complications. Although there was no difference in major complications of thyroidectomy, it should be noted that there was an increased risk of minor complications, defined as temporary RLN injury, temporary hypoparathyroidism, seroma formation, skin infection, and mental nerve injury. The risk of minor complications such as these was 17.5% in the TOETVA group compared to 9.3% the TCA group (P=0.007) (21). Table 2 details the complication rates in recently published case series within our inclusion criteria. However, there is a continued decrease in complication rates over time and surgeon experience, with improvement in outcomes seen well past the learning curve period (46,47).
Table 2
| First author, year |
N | Extent of surgery | Temporary RLN injury‡ | Permanent RLN injury‡ | Temporary HPT* | Permanent HPT* | Temporary MNI | Permanent MNI | Infection | Hematoma | Soft tissue injury |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ahn, 2020 (34) |
150 | 40 TT; 10 HT |
7 (3.7%) | 1 (0.5%) | 5 (12.5%) | 2 (5.0%) | 0 | 0 | 0 | 1 (0.7%) | – |
| Dinc, 2020 (24) |
56 | 43 TT; 13 HT |
2 (2.0%) | 0 | 10 (17.8%) | 0 | 0 | 0 | 3 (5.4%) | – | 2 (3.6%) |
| Fernandez Ranvier, 2020 (29) | 152 | 38 TT; 111 HT; 3 CT |
5 (2.6%) | 3 (1.6%) | 7 (17.1%) | 0 | 28 (18.4%) | 1 (0.7%) | 1 (0.7%) | 3 (2.0%) | 9 (5.9%) |
| Fernandez-Ranvier, 2020 (35) | 50 | 12 TT; 38 HT |
2 (3.2%) | 1 (1.6%) | 1 (8.3%) | 0 | 29 (58.0%) | 1 (2.0%) | – | – | 4 (8.0%) |
| Hong, 2020 (36) |
82 | 12 TT; 70 HT |
3 (3.2%) | 0 | 1 (8.3%) | 0 | – | 0 | 2 (2.4%) | 0 | 0 |
| Kim, 2020 (37) |
132 | 8 TT; 124 HT |
6 (4.3%) | 0 | 1 (12.5%) | 0 | 2 (1.5%) | 1 (0.8%) | 1 (0.8%) | 1 (0.8%) | – |
| Lira, 2020 (28) |
56 | 37 TT; 19 HT |
2 (2.1%) | 0 | 4 (10.8%) | 0 | 0 | 0 | 1 (1.8%) | 0 | 0 |
| Luna-Ortiz, 2020 (38) | 46 | 44 TT; 2 HT |
1 (1.1%) | 2 (2.2%) | – | 2 (4.5%) | 0 | 0 | – | – | – |
| Peng, 2020 (39) |
105 | 10 TT; 95 HT |
3 (2.6%) | 2 (1.7%) | 2 (20.0%) | 0 | 3 (2.9%) | 0 | 1 (0.8%) | – | – |
| Alsafran, 2021 (40) | 4 | 0 TT; 4 HT |
0 | 0 | 0 | 0 | 1 (25.0%) | 0 | 0 | 0 | – |
| Chai, 2021 (20) |
110 | 3 TT; 100 HT; 7 Isth |
5 (4.4%) | 1 (0.9%) | 1 (33.3%) | 0 | 0 | 0 | 0 | 1 (0.9%) | – |
| Deroide, 2021 (41) | 90 | 41 TT; 44 HT; 5 Isth |
7 (5.3%) | 0 | 8 (19.5%) | 0 | 26 (28.9%) | 1 (1.1%) | 0 | 0 | 1 (1.1%) |
| Lira, 2021 (42) |
412 | 265 TT; 144 HT; 3 Isth |
30 (4.4%) | 4 (0.6%) | 19 (7.2%) | 3 (1.1%) | 7 (1.7%) | 0 | 1 (0.2%) | 2 (0.5%) | 8 (1.9%) |
| Nguyen, 2022 (43) | 326 | 47 TT; 279 HT |
9 (2.4%) | 0 | 12 (25.5%) | 0 | 7 (2.1%) | 0 | 0 | – | – |
| Russell, 2021 (21) | 200 | 36 TT; 159 HT; 5 CT |
9 (3.3%) | 0 | 14 (18.2%) | 0 | – | 5 (2.5%) | 2 (1.0%) | 0 | 2 (1%) |
| Zheng, 2021 (44) | 297 | 10 TT; 287 HT |
4 (1.3%) | 4 (1.3%) | 3 (30.0%) | 0 | 234 (78.8%) | 7 (2.4%) | 2 (0.6%) | 0 | – |
| Yap, 2022 (45) |
9 | 9 TT; 0 HT |
0 | 0 | 3 (33.3%) | 2 (22.2%) | 2 (22.2%) | 0 | 0 | 0 | – |
‡, rates of recurrent laryngeal nerve injury calculated for total number of nerves at risk. *, hypoparathyroidism as defined by each study. Rates of transient or permanent hypoparathyroidism calculated only for total thyroidectomy and completion thyroidectomy cases. N, number; RLN, recurrent laryngeal nerve; HPT, hypoparathyroidism; MNI, mental nerve injury; TT, total thyroidectomy; HT, hemithyroidectomy; CT, completion thyroidectomy; Isth, isthmusectomy.
In TOETVA, dissection of the RLN differs from the technique in open surgery. Cranial to caudal dissection is necessary, as the nerve is encountered first at its entrance into the laryngeal musculature. In a series of 145 TOETVA patients, Zhang et al. found that the majority (58%) of nerve injuries were thermal and occurred during dissection at the ligament of Berry (48). This is in contrast to several other studies examining mechanism of nerve injury in TCA, which were more commonly traction or compression injuries (49,50). Thermal injuries were found to have a longer recovery period than other methods of injury. It is possible that there is more thermal spread with the hemostatic instruments used in TOETVA compared to TCA. This information is critical for operating surgeons to be cognizant of in order to avoid excessive thermal instrumentation at the ligament of Berry and reduce the risk of nerve injury.
Another complication that may arise due to anatomic differences in how the gland is accessed during surgery is injury to the mental nerve. The mental nerve exits the mental foramen in the mandible and divides into three branches, providing sensory innervation to the chin and lower lip. Branches of the mental nerve can be at risk of injury in TOETVA during trocar placement in the oral vestibule, particularly the lateral ports. In Russell et al.’s review, there was a 2.5% (n=5) incidence of permanent mental nerve injury, defined as hypoesthesia persisting greater than 6 months (21). The incidence of transient mental nerve hypoesthesia is far more reported, with Zheng et al. documenting varying degrees of mental nerve disturbance in 81.1% of their 297 TOETVA patients, with only 2.4% of all patients experiencing permanent mental dysesthesia (44). In addition, 12 of their patients (4.0%) experienced abnormal motor function of the lower lip and chin, all of which had resolved by 12 month follow up.
Minimizing the risk and degree of mental nerve injury or paresthesia has been a goal of surgeons since the advent of TOETVA, with Anuwong and Kim both providing modifications of port placement in 2018 (51,52) from the initially described technique (4). In 2021, Zheng et al. provided further modifications with the aim of reducing sensory and motor changes in the mental nerve distribution by proposing an arc-shaped middle mucosal incision and lateral incisions near the oral commissure adjacent to the mucosal folds (53). In the group utilizing the original incision design (Group A, n=39), 100% had sensory alterations of the lip and chin immediately post operatively, compared with 79.5% of the patients with the altered incision (Group B, n=83). The time to recovery of these changes was significantly longer in the first group (4.5±3.1 months) compared to the second (1.9±1.3 months, P<0.001). Complete recovery of these sensory changes at 12 months occurred in only 56.4% of Group A, compared to 97.0% of Group B. In terms of motor outcomes, 23.1% of patients in Group A had abnormal motor function of the lip and chin post operatively, including pronunciation changes, abnormal appearance during smiling, and liquid leakage while eating or drinking. In Group B, only 2.4% of patients experienced these changes. It should be noted that in both groups these motor changes resolved by 12 months, although the time to resolution was longer for Group A (53).
As evidenced by these studies, there is a wide range in the reported incidence of mental nerve injury. This may be in part due to differing definitions of true mental nerve injury, as some authors may ascribe all post-operative sensory changes to the mental area as an injury while others account only for cases with severe sensory loss. When Tae et al. prospectively evaluated multiple cutaneous zones of the face using a Semmes-Weinstein monofilament in 43 patients, they found that the pressure thresholds of the chin and lower lip had no significant post-operative change compared to preoperative baseline, and that there were no cases of true mental nerve injury on objective measure (54). This data suggests that varying definitions for mental nerve injury among physicians may account for the discrepancy reported in the literature, and that the incidence of true mental nerve injury is rare.
Another novel complication with TOETVA is the risk of flap perforation or skin burn, which may occur with placement of the ports or during flap creation (55). Although the incidence is not consistently reported in all studies, Table 2 demonstrates that this complication occurred in 0–8.0% of published cases. Other soft tissue effects of skin dimpling, tissue tethering, or a “pulling” sensation have also been reported in the literature (28,55). While seemingly rare, these alterations in appearance may be significant in a population highly motivated to avoid visible evidence of their surgery.
Given the intra-oral access to the surgical field, the risk of post-operative infection is another variable to consider in TOETVA. While TCA thyroid surgery is deemed a “clean” procedure with no prophylactic antibiotics indicated (56), procedures involving the oral vestibule are “clean-contaminated”. Therefore, antibiotic prophylaxis pre-procedure is generally recommended, with many continuing coverage for 3–7 days post operatively (4,15,52,57). However, other more recently published series have found no increased rate of infection over TCA even without extended antibiotic prophylaxis (20,58). Overall, in comparison with TCA, vestibular access does not seem have an increased rate of infection (52,58-60). A large meta-analysis completed in 2022 concurs, with only a 0.64% infection rate in the 1,887 patients studied (61).
While nodule disruption during removal is not necessarily thought of as a complication of the procedure, such an occurrence can violate oncologic principles and make assessment of capsular involvement and extrathyroidal extension difficult. Several studies have examined rates of capsular disruption on final pathology. Wu et al. found that a nodule diameter of 20 mm had a 100% sensitivity and 87% specificity for remaining intact on final pathology (18). Likewise, Smith et al. found a median nodule size of 19 mm when examining unruptured nodules (62). In both studies, there was a significant capsule disruption rate [59% (18) and 68% (62)] when considering all sizes of nodules removed. For this reason, it is imperative that surgeons adhere to published size guidelines when considering malignant or suspicious nodules for TOETVA to ensure accurate pathologic analysis. Some surgeons have combined TOETVA with other remote access incisions (submental, axillary, retro-auricular) in order to allow the benefits of a laparoscopic TOETVA dissection with a larger port for thyroid removal, allowing for larger specimens to be removed in this manner (58,63,64).
Operating time
Despite increases in implementation and increasing case volumes, TOETVA has longer operating times than the traditional approach. In Russell et al.’s review, the median operative time for a TOETVA lobectomy vs. TCA lobectomy was 123 minutes compared to 75 minutes respectively (P=0.001) (21). A TOETVA total thyroidectomy was 184 minutes, and TCA total thyroidectomy was 116 minutes (P=0.001). Similarly, de Vries et al. found a significant difference between the two methods, with the operating times of 152 vs. 105.5 minutes for TOETVA and TCA respectively (33). Although this time decreases with increased case experience (28,43), there remains a significant difference in time (28,32,65), albeit less than a robotic approach (66). Table 3 details the published operative times of TOETVA lobectomy and thyroidectomy compared to TCA.
Table 3
| First author, year | TOETVA lobectomy (min) | TOETVA TT (min) | TCA lobectomy (min) | TCA TT (min) |
|---|---|---|---|---|
| Ahn, 2020 (34) | 102.1 | 143.6 | 76.4 | 90.7 |
| Fernandez Ranvier, 2020 (29) | 161.8 | 213.4 | – | – |
| Fernandez-Ranvier, 2020 (35) | 149.0 | 217.6 | – | – |
| Hong, 2020 (36) | 112.3 | 155.9 | 59.5 | 79.8 |
| Alsafran, 2021 (40) | 151.0 | – | – | – |
| Chai, 2021 (20) | 110.0 | 168.0 | – | – |
| Deroide, 2021 (41) | 120.6 | 168 | – | – |
| Nguyen, 2022 (43) | 90.7 | 113.4 | – | – |
| Razavi, 2021 (65) | 127 | 176 | 92 | 125 |
| Russell, 2021 (21) | 123 | 184 | 75 | 116 |
| Zheng, 2021 (44) | 135.6 | 189.3 | – | – |
TOETVA, transoral endoscopic thyroidectomy vestibular approach; TT, total thyroidectomy; TCA, transcervical approach; min, minutes.
Cost
Operative time also has an influence on the cost of the procedure. The first study of its kind was published in 2021 by Razavi et al. which examined the direct cost of TOETVA as well as time-independent costs (65). One hundred and eighteen patients underwent TOETVA and 120 underwent TCA at the same institution by the same two experienced endocrine surgeons. The mean variable direct cost was $4,455 USD (SD 1,129, 95% CI: 4,204–4,706) for TOETVA lobectomy compared to $3,179 USD (SD 687, 95% CI: 2,990–3,369) for TCA lobectomy (P<0.001). Independent of time, the mean cost for TOETVA lobectomy was $3,370 USD (SD 974, 95% CI: 3,154–3,587) compared to $2,409 USD (SD 550, 95% CI: 2,257–2,560) for TCA lobectomy (P<0.001). Although TOETVA is a more costly procedure independent of operating time, the difference in energy devices alone contributed nearly $500 USD (38.2% and 43.2%) of the cost difference for lobectomies and total thyroidectomies, respectively. Although energy devices are commonly used in both TCA and TOETVA procedures, this institution used different instruments for each procedure, which accounted for the cost difference referenced in that study. The total difference in cost between TOETVA and TCA is considerably less than previously reported for robotic thyroidectomies (67) and is certainly an important factor in the continued implementation of TOETVA across institutions that offer remote access techniques.
Learning curve
As with any procedural skill, the time it takes to complete a task is expected to decrease with provider skill and experience. The learning curve for TOETVA is estimated in some series to be approximately 11–15 cases (28,68), whereas others have found proficiency can take up to 50–60 cases (20,69,70). It is critical that surgeons are aware of the possible intra-operative difficulties and complications that can arise during a novel procedure. For this reason, it is recommended that extensive preparation occurs prior to implementing TOETVA in one’s practice. This preparation includes ensuring high thyroid volume, familiarity with existing literature, operative team/administration preparation, familiarity with the procedure, real-time observation of cases, cadaver dissection, and preceptor presence for initial cases (71). Careful patient selection is also critical during the learning curve, with consideration of the benefit to each patient in order to achieve optimal outcomes and limit complications. Informed consent must be obtained regarding the novel nature of this approach with the discussion of potential complications (71). With these steps in place, several series detailing their initial experience with TOETVA even during their learning curve have demonstrated acceptable outcomes (21,28,31,34,40,41,70).
Disease-related outcomes
Finally, efficacy in disease-directed treatment is a critical element to examine. Liu et al. published a propensity score-matched analysis of outcomes in patients with papillary thyroid cancer measuring 1.0–3.5 cm (72). While they too had equivalent complication rates between the groups in line with the other papers discussed, they also examined the number of lymph nodes harvested and post-operative thyroglobulin (Tg) levels between the two groups. They found that there was no difference in the median number of central lymph nodes harvested (9 vs. 10, P=0.154) or the rate of lymph nodes metastasis (69.2% vs. 71.8%, P=0.725) between the TOETVA and TCA groups respectively. Additionally, there was no significant difference in the median stimulated Tg level (0.50 vs. 0.99 µg/L, P=0.118) and the percentage of patients with an unstimulated Tg level <1.0 µg/L (61.9% vs. 50.0%, P=0.423). While Zheng et al. did not compare their outcomes to a TCA control group, they too harvested a mean 6.6±4.1 (lobectomy) and 10.9±4.0 (total thyroidectomy) lymph nodes, with non-stimulated Tg levels in the total thyroidectomy group below 1 ng/mL at 6 months (44). These studies demonstrate appropriate oncologic clearance can be performed with TOETVA, and that malignancy (with appropriate patient selection) should not be a deterrent to the procedure. Although data does not yet exist for long term oncologic outcomes, short term recurrence rates are promising (43).
Conclusions
The TOETVA literature published in 2020–2022 includes data from several large case series and meta-analysis. There has been increased performance of this procedure by surgeons and pursual by patients, evidenced by the more proliferative publication and adoption of this method compared to other remote access approaches. The recently published literature further illustrates TOETVA as a safe method in patients who are motivated to avoid a cervical incision. It must be noted that while these recent studies demonstrate equivalence in major complications, there is a higher published rate of minor complications with TOETVA. Careful and appropriate patient selection remains paramount to maximize patient safety and optimize outcomes. This remains true in cases of malignancy, although there has been no difference found in short-term oncologic outcomes between TOETVA and TCA. While this is a safe and effective surgical method, the increased operative time and higher costs may hinder implementation in some practices. Further prospective research comparing quality of life and long-term disease-related outcomes between the traditional approach and TOETVA are warranted to ensure optimal patient and disease-directed outcomes.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Ralph P. Tufano and Salem I. Noureldine) for the series “Novel Technology and Techniques in the Management of Thyroid Nodules” published in Annals of Thyroid. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://aot.amegroups.com/article/view/10.21037/aot-22-5/rc
Peer Review File: Available at https://aot.amegroups.com/article/view/10.21037/aot-22-5/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://aot.amegroups.com/article/view/10.21037/aot-22-5/coif). The series “Novel Technology and Techniques in the Management of Thyroid Nodules” was commissioned by the editorial office without any funding or sponsorship. SAW has received reimbursement from her employing institution for conference fees and travel costs to present research. JOR is a consultant for Baxter scientific, and has also received honoraria for speaking and payment for expert testimony. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wilhelm T, Harlaar JJ, Kerver A, et al. Surgical anatomy of the floor of the oral cavity and the cervical spaces as a rationale for trans-oral, minimal-invasive endoscopic surgical procedures: results of anatomical studies. Eur Arch Otorhinolaryngol 2010;267:1285-90. [Crossref] [PubMed]
- Wilhelm T, Metzig A. Video. Endoscopic minimally invasive thyroidectomy: first clinical experience. Surg Endosc 2010;24:1757-8. [Crossref] [PubMed]
- Yang J, Wang C, Li J, et al. Complete Endoscopic Thyroidectomy via Oral Vestibular Approach Versus Areola Approach for Treatment of Thyroid Diseases. J Laparoendosc Adv Surg Tech A 2015;25:470-6. [Crossref] [PubMed]
- Anuwong A. Transoral Endoscopic Thyroidectomy Vestibular Approach: A Series of the First 60 Human Cases. World J Surg 2016;40:491-7. [Crossref] [PubMed]
- Russell JO, Sahli ZT, Shaear M, et al. Transoral thyroid and parathyroid surgery via the vestibular approach-a 2020 update. Gland Surg 2020;9:409-16. [Crossref] [PubMed]
- Banuchi VE, Ballakur SS, Russell JO, et al. Benefits and risks of scarless thyroid surgery. Ann Thyroid 2020; [Crossref]
- Dionigi G, Tufano RP, Russell J, et al. Transoral thyroidectomy: advantages and limitations. J Endocrinol Invest 2017;40:1259-63. [Crossref] [PubMed]
- Arora A, Swords C, Garas G, et al. The perception of scar cosmesis following thyroid and parathyroid surgery: A prospective cohort study. Int J Surg 2016;25:38-43. [PubMed]
- Goswami S, Peipert BJ, Mongelli MN, et al. Clinical factors associated with worse quality-of-life scores in United States thyroid cancer survivors. Surgery 2019;166:69-74. [Crossref] [PubMed]
- Juarez MC, Ishii L, Nellis JC, et al. Objectively measuring social attention of thyroid neck scars and transoral surgery using eye tracking. Laryngoscope 2019;129:2789-94. [Crossref] [PubMed]
- Liao D, Ishii LE, Chen LW, et al. Transoral neck surgery prevents attentional bias towards the neck compared to open neck surgery. Laryngoscope 2020;130:1603-8. [Crossref] [PubMed]
- Choi Y, Lee JH, Kim YH, et al. Impact of postthyroidectomy scar on the quality of life of thyroid cancer patients. Ann Dermatol 2014;26:693-9. [Crossref] [PubMed]
- Sethukumar P, Ly D, Awad Z, et al. Scar satisfaction and body image in thyroidectomy patients: prospective study in a tertiary referral centre. J Laryngol Otol 2018;132:60-7. [Crossref] [PubMed]
- Grogan RH, Suh I, Chomsky-Higgins K, et al. Patient Eligibility for Transoral Endocrine Surgery Procedures in the United States. JAMA Netw Open 2019;2:e194829. [Crossref] [PubMed]
- Jitpratoom P, Ketwong K, Sasanakietkul T, et al. Transoral endoscopic thyroidectomy vestibular approach (TOETVA) for Graves' disease: a comparison of surgical results with open thyroidectomy. Gland Surg 2016;5:546-52. [Crossref] [PubMed]
- Russell JO, Clark J, Noureldine SI, et al. Transoral thyroidectomy and parathyroidectomy - A North American series of robotic and endoscopic transoral approaches to the central neck. Oral Oncol 2017;71:75-80. [Crossref] [PubMed]
- Wang C, Zhai H, Liu W, et al. Thyroidectomy: a novel endoscopic oral vestibular approach. Surgery 2014;155:33-8. [Crossref] [PubMed]
- Wu YJ, Chi SY, Elsarawy A, et al. What is the Appropriate Nodular Diameter in Thyroid Cancer for Extraction by Transoral Endoscopic Thyroidectomy Vestibular Approach Without Breaking the Specimens? A Surgicopathologic Study. Surg Laparosc Endosc Percutan Tech 2018;28:390-3. [Crossref] [PubMed]
- Razavi CR, Russell JO. Indications and contraindications to transoral thyroidectomy. Ann Thyroid 2017;2:12. [Crossref] [PubMed]
- Chai YJ, Chae S, Oh MY, et al. Transoral Endoscopic Thyroidectomy Vestibular Approach (TOETVA): Surgical Outcomes and Learning Curve. J Clin Med 2021;10:863. [Crossref] [PubMed]
- Russell JO, Razavi CR, Shaear M, et al. Transoral Thyroidectomy: Safety and Outcomes of 200 Consecutive North American Cases. World J Surg 2021;45:774-81. [Crossref] [PubMed]
- Tufano RP, Mohamed Ali K. The Year in Surgical Thyroidology: Recent Technological Developments and Future Challenges. Thyroid 2022;32:14-8. [Crossref] [PubMed]
- Tai DKC, Kim HY, Park D, et al. Obesity May Not Affect Outcomes of Transoral Robotic Thyroidectomy: Subset Analysis of 304 Patients. Laryngoscope 2020;130:1343-8. [Crossref] [PubMed]
- Dinc B, Gunduz UR, Belen NH. Transoral Endoscopic Thyroidectomy Vestibular Approach (TOETVA) in Thyroiditis. Surg Laparosc Endosc Percutan Tech 2020;31:188-92. [Crossref] [PubMed]
- Miller KD, Fidler-Benaoudia M, Keegan TH, et al. Cancer statistics for adolescents and young adults, 2020. CA Cancer J Clin 2020;70:443-59. [Crossref] [PubMed]
- Fassas S, Mamidi I, Lee R, et al. Postoperative Complications After Thyroidectomy: Time Course and Incidence Before Discharge. J Surg Res 2021;260:210-9. [Crossref] [PubMed]
- Brauer PR, Reddy CA, Burkey BB, et al. A National Comparison of Postoperative Outcomes in Completion Thyroidectomy and Total Thyroidectomy. Otolaryngol Head Neck Surg 2021;164:566-73. [Crossref] [PubMed]
- Lira RB, Ramos AT, Nogueira RMR, et al. Transoral thyroidectomy (TOETVA): Complications, surgical time and learning curve. Oral Oncol 2020;110:104871. [Crossref] [PubMed]
- Fernandez Ranvier G, Meknat A, Guevara DE, et al. International Multi-institutional Experience with the Transoral Endoscopic Thyroidectomy Vestibular Approach. J Laparoendosc Adv Surg Tech A 2020;30:278-83. [Crossref] [PubMed]
- Russell JO, Razavi CR, Garstka ME, et al. Remote-Access Thyroidectomy: A Multi-Institutional North American Experience with Transaxillary, Robotic Facelift, and Transoral Endoscopic Vestibular Approaches. J Am Coll Surg 2019;228:516-22. [Crossref] [PubMed]
- Pérez-Soto RH, Ponce de León-Ballesteros G, Montalvo-Hernández J, et al. Transoral Endoscopic Thyroidectomy by Vestibular Approach-Initial Experience and Comparative Analysis in the First Reported Mexican Cohort. J Laparoendosc Adv Surg Tech A 2019;29:1526-31. [Crossref] [PubMed]
- Wang Y, Zhou S, Liu X, et al. Transoral endoscopic thyroidectomy vestibular approach vs conventional open thyroidectomy: Meta-analysis. Head Neck 2021;43:345-53. [Crossref] [PubMed]
- de Vries LH, Aykan D, Lodewijk L, et al. Outcomes of Minimally Invasive Thyroid Surgery - A Systematic Review and Meta-Analysis. Front Endocrinol (Lausanne) 2021;12:719397. [Crossref] [PubMed]
- Ahn JH, Yi JW. Transoral endoscopic thyroidectomy for thyroid carcinoma: outcomes and surgical completeness in 150 single-surgeon cases. Surg Endosc 2020;34:861-7. [Crossref] [PubMed]
- Fernandez-Ranvier G, Meknat A, Guevara D, et al. Transoral Endoscopic Thyroidectomy Vestibular Approach: A Single-institution Experience of the First 50 Cases. Surg Innov 2020;27:439-44. [Crossref] [PubMed]
- Hong YT, Ahn JH, Kim JH, et al. Bi-institutional experience of transoral endoscopic thyroidectomy: Challenges and outcomes. Head Neck 2020;42:2115-22. [Crossref] [PubMed]
- Kim SY, Kim SM, Makay Ö, et al. Transoral endoscopic thyroidectomy using the vestibular approach with an endoscopic retractor in thyroid cancer: experience with the first 132 patients. Surg Endosc 2020;34:5414-20. [Crossref] [PubMed]
- Luna-Ortiz K, Gómez-Pedraza A, Anuwong A. Lessons Learned from the Transoral Endoscopic Thyroidectomy with Vestibular Approach (TOETVA) for the Treatment of Thyroid Carcinoma. Ann Surg Oncol 2020;27:1356-60. [Crossref] [PubMed]
- Peng X, Li Z, Li H, et al. The clinical application of mental nerve dissection in transoral endoscopic thyroidectomy via an oral vestibular approach. Surg Endosc 2020;34:153-8. [Crossref] [PubMed]
- Alsafran S, Quttaineh D, Albloushi D, et al. Trans-oral endoscopic endocrine surgery vestibular approach: Pioneering the technique in the Gulf Cooperation Council Countries - A case series. Ann Med Surg (Lond) 2021;72:103114. [Crossref] [PubMed]
- Deroide G, Honigman I, Berthe A, et al. Trans oral endoscopic thyroidectomy (TOETVA): First French experience in 90 patients. J Visc Surg 2021;158:103-10. [Crossref] [PubMed]
- Lira RB, De Cicco R, Rangel LG, et al. Transoral endoscopic thyroidectomy vestibular approach: Experience from a multicenter national group with 412 patients. Head Neck 2021;43:3468-75. [Crossref] [PubMed]
- Nguyen HX, Nguyen HX, Nguyen TTP, et al. Transoral endoscopic thyroidectomy by vestibular approach in Viet Nam: surgical outcomes and long-term follow-up. Surg Endosc 2022;36:4248-54. [Crossref] [PubMed]
- Zheng G, Ma C, Sun H, et al. Safety and surgical outcomes of transoral endoscopic thyroidectomy vestibular approach for papillary thyroid cancer: A two-centre study. Eur J Surg Oncol 2021;47:1346-51. [Crossref] [PubMed]
- Yap RV, Villamor M Jr. Scarless total thyroidectomy via transoral endoscopic vestibular approach: initial case series in a developing Asian country. J Surg Case Rep 2022;2022:rjab623. [Crossref] [PubMed]
- Kuo TC, Duh QY, Wang YC, et al. Practice Patterns and Learning Curve in Transoral Endoscopic Thyroidectomy Vestibular Approach With Neuromonitoring. Front Endocrinol (Lausanne) 2021;12:744359. [Crossref] [PubMed]
- Trakimas DR, Wolfe SA, Razavi CR, et al. Safety & outcomes of 341 consecutive transoral endoscopic thyroidectomy vestibular approach cases in North America Presented at: AHNS at COSM; April 28, 2022; Dallas, TX, USA.
- Zhang D, Sun H, Tufano R, et al. Recurrent laryngeal nerve management in transoral endoscopic thyroidectomy. Oral Oncol 2020;108:104755. [Crossref] [PubMed]
- Chiang FY, Lu IC, Kuo WR, et al. The mechanism of recurrent laryngeal nerve injury during thyroid surgery--the application of intraoperative neuromonitoring. Surgery 2008;143:743-9. [Crossref] [PubMed]
- Snyder SK, Lairmore TC, Hendricks JC, et al. Elucidating mechanisms of recurrent laryngeal nerve injury during thyroidectomy and parathyroidectomy. J Am Coll Surg 2008;206:123-30. [Crossref] [PubMed]
- Kim HY, Chai YJ, Dionigi G, et al. Transoral robotic thyroidectomy: lessons learned from an initial consecutive series of 24 patients. Surg Endosc 2018;32:688-94. [Crossref] [PubMed]
- Anuwong A, Sasanakietkul T, Jitpratoom P, et al. Transoral endoscopic thyroidectomy vestibular approach (TOETVA): indications, techniques and results. Surg Endosc 2018;32:456-65. [Crossref] [PubMed]
- Zheng G, Wang X, Wu G, et al. The sensorimotor changes of the lower lip and chin after transoral endoscopic thyroidectomy vestibular approach. Updates Surg 2021;73:2283-91. [Crossref] [PubMed]
- Tae K, Lee DW, Bang HS, et al. Sensory change in the chin and neck after transoral thyroidectomy: Prospective study of mental nerve injury. Head Neck 2020;42:3111-7. [Crossref] [PubMed]
- Bakkar S, Al Hyari M, Naghawi M, et al. Transoral thyroidectomy: a viable surgical option with unprecedented complications-a case series. J Endocrinol Invest 2018;41:809-13. [Crossref] [PubMed]
- Polistena A, Prete FP, Avenia S, et al. Effect of Antibiotic Prophylaxis on Surgical Site Infection in Thyroid and Parathyroid Surgery: A Systematic Review and Meta-Analysis. Antibiotics (Basel) 2022;11:290. [Crossref] [PubMed]
- Dionigi G, Lavazza M, Bacuzzi A, et al. Transoral Endoscopic Thyroidectomy Vestibular Approach (TOETVA): From A to Z. Surg Technol Int 2017;30:103-12. [PubMed]
- Karakas E, Klein G, Michlmayr L, et al. Transoral thyroid surgery vestibular approach: is there an increased risk of surgical site infections? Updates Surg 2022;74:303-8. [Crossref] [PubMed]
- Camenzuli C, Schembri Wismayer P, Calleja Agius J. Transoral Endoscopic Thyroidectomy: A Systematic Review of the Practice So Far. JSLS 2018;22:e2018. [Crossref] [PubMed]
- Shan L, Liu J. A Systemic Review of Transoral Thyroidectomy. Surg Laparosc Endosc Percutan Tech 2018;28:135-8. [Crossref] [PubMed]
- Akritidou E, Douridas G, Spartalis E, et al. Complications of Trans-oral Endoscopic Thyroidectomy Vestibular Approach: A Systematic Review. In Vivo 2022;36:1-12. [Crossref] [PubMed]
- Smith SM, Ahmed M, Carling T, et al. Impact of Transoral Endoscopic Vestibular Approach Thyroidectomy on Pathologic Assessment. Arch Pathol Lab Med 2022;146:879-85. [Crossref] [PubMed]
- Karakas E, Klein G, Schopf S. Transoral thyroid surgery vestibular approach: does size matter anymore? J Endocrinol Invest 2020;43:615-22. [Crossref] [PubMed]
- Chen Y, Chomsky-Higgins K, Nwaogu I, et al. Hidden in Plain Sight: Transoral and Submental Thyroidectomy as a Compelling Alternative to "Scarless" Thyroidectomy. J Laparoendosc Adv Surg Tech A 2018;28:1374-7. [Crossref] [PubMed]
- Razavi CR, Tanavde VA, Kim AS, et al. The variable direct cost and cost drivers of transoral endoscopic thyroidectomy vestibular approach. Gland Surg 2021;10:521-8. [Crossref] [PubMed]
- Chen YH, Kim HY, Anuwong A, et al. Transoral robotic thyroidectomy versus transoral endoscopic thyroidectomy: a propensity-score-matched analysis of surgical outcomes. Surg Endosc 2021;35:6179-89. [Crossref] [PubMed]
- Broome JT, Pomeroy S, Solorzano CC. Expense of robotic thyroidectomy: a cost analysis at a single institution. Arch Surg 2012;147:1102-6. [Crossref] [PubMed]
- Razavi CR, Vasiliou E, Tufano RP, et al. Learning Curve for Transoral Endoscopic Thyroid Lobectomy. Otolaryngol Head Neck Surg 2018;159:625-9. [Crossref] [PubMed]
- Lee J, Lee JH, Nah KY, et al. Comparison of endoscopic and robotic thyroidectomy. Ann Surg Oncol 2011;18:1439-46. [Crossref] [PubMed]
- Luo JH, Xiang C, Wang P, et al. The Learning Curve for Transoral Endoscopic Thyroid Surgery: A Single Surgeon's 204 Case Experience. J Laparoendosc Adv Surg Tech A 2020;30:163-9. [Crossref] [PubMed]
- Russell JO, Anuwong A, Dionigi G, et al. Transoral Thyroid and Parathyroid Surgery Vestibular Approach: A Framework for Assessment and Safe Exploration. Thyroid 2018;28:825-9. [Crossref] [PubMed]
- Liu Z, Li Y, Wang Y, et al. Comparison of the transoral endoscopic thyroidectomy vestibular approach and open thyroidectomy: A propensity score-matched analysis of surgical outcomes and safety in the treatment of papillary thyroid carcinoma. Surgery 2021;170:1680-6. [Crossref] [PubMed]
Cite this article as: Wolfe SA, Russell JO. A narrative review of transoral thyroidectomy—2021 update. Ann Thyroid 2022;7:12.