
Incidental diagnosis of ectopic thyroid in the work-up of metastatic esophageal cancer: a case report
Introduction
The incidence of ectopic thyroid is rare and has been reported to be between 1/100,000 to 1/300,000 (1,2). Although the exact pathophysiology is unknown, ectopic thyroid is believed to occur from abnormal deviation of thyroid tissue from its normal migrational path during the 7th embryological week (3,4). Distributional data from various studies demonstrate that ectopic thyroid occurs more commonly in medial structures such as lingual, thyroglossal, laryngeal and tracheal sites, and less commonly in lateral structures such as esophageal, aortic, mediastinal and pancreatic areas (3,5). Most ectopic thyroid has been reported to be benign, while malignant ectopic thyroid appears to comprise less than 1% of all cases (1). While encountering a case of ectopic thyroid is by itself a rare occurence, the detection of benign ectopic thyroid tissue via fluorodeoxyglucose-positron emission tomography-computerized tomography (FDG-PET-CT) scan is even rarer. We present a case of FDG-avid ectopic thyroid that was suspected to be a metastatic supraclavicular lymph node in a patient with known esophageal cancer. From our knowledge, this may be one of the very few if not the only case of FDG avid benign ectopic thyroid discovered in the workup of esophageal malignancy. We present the following case in accordance with the CARE reporting checklist (available at https://aot.amegroups.com/article/view/10.21037/aot-21-24/rc).
Case presentation
A 76-year-old male patient with no notable past medical history was evaluated at the outpatient primary care office for 1 month of progressively worsening dysphagia. To further investigate the etiology of these symptoms, the patient was recommended to undergo esophagogastroduodenoscopy (EGD) which showed an exophytic mass at the gastroesophageal (GE) junction. Biopsy of the mass confirmed moderately to poorly differentiated invasive adenocarcinoma, prompting referral to the oncology clinic for further management. There was no medical history of hematologic, thyroid or gastrointestinal malignancy in the patient’s family. Patient was a non-smoker with no documentation of radiation history. Physical exam revealed no hoarseness, no abdominal tenderness, no neck swelling and tenderness, and no palpable lymph nodes or masses in cervical and supraclavicular region.
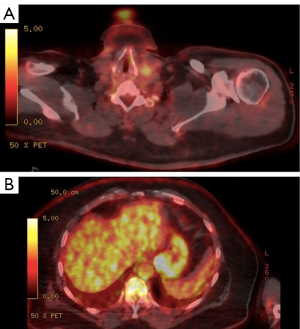
For staging, patient was asked to undergo a FDG-PET-CT scan at our radiology department (Figure 1). On PET-CT, a hypermetabolic FDG-avid focus with maximum standardized uptake value (SUVmax) of 24.0 was identified at the GE junction, which correlated well with the patient’s known primary tumor (Figure 1B). In addition, PET-CT showed a mild hypermetabolic focus measuring 2.2×2.1 cm with a SUVmax of 3.4 in the left supraclavicular region (Figure 1A). This was suspected to represent metastatic spread of esophageal cancer. The frequency of supraclavicular lymph node metastases from lower esophageal tumor has been reported to be 9.3% (6).
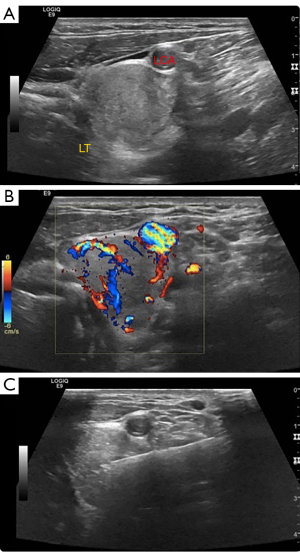
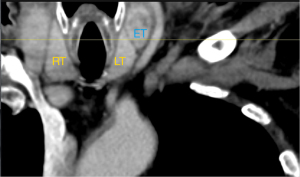
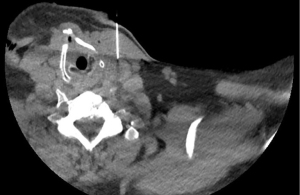
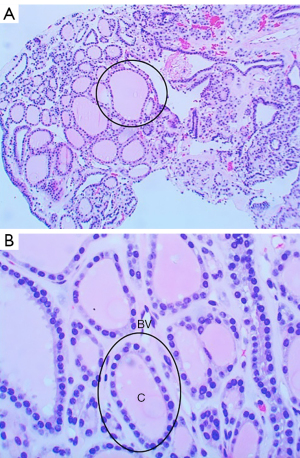
Patient was sent for ultrasound-guided biopsy (Figure 2) to determine the identity of the supraclavicular PET avid lesion, which demonstrated benign thyroid tissue on microscopic analysis. Given the close relation of the biopsy target to the left thyroid lobe as shown on the coronal post-contrast CT scan (Figure 3), the possibility of non-targeted biopsy was considered. CT-guided re-biopsy was carried out (Figure 4), which again showed benign thyroid tissue (Figure 5). Patient tolerated both biopsy procedures well with no complications. No further intervention was proceeded on these findings and the patient was referred to surgery for further management of esophageal cancer. All procedures performed in studies were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Ectopic thyroid is defined as thyroid tissue found outside of the normal anatomic location of the thyroid gland (7). Thyroid gland derives from the endodermal tissue and initiates its migratory pathway from the foramen cecum (1,2). Under normal embryological process, thyroid gland descends as the bi-lobed diverticulum from the foramen cecum to the anterior of hyoid bone (2). By 7th gestational week, thyroid gland reaches its anatomic destination at upper trachea, anterior to the 2nd to 4th tracheal rings, posterior to the sternothyroid and sternohyoid muscles and inferior to the laryngeal thyroid cartilage (2,4). An exact etiology for the formation of ectopic thyroid has not been well studied. Studies have shown that ectopic thyroid have been found in both medial and peripheral structures including submandibular, sublingual, laryngeal, esophageal, cervical, mediastinal, pericardial, and aortic sites (3,4). The prevalence of ectopic thyroid ranges from 1/100,000 to 1/300,000 (1,2).
While encountering ectopic thyroid outside the normal anatomic location itself is rare, detection of benign ectopic thyroid via FDG-PET-CT scan is even rarer. We present a very rare finding of FDG-avid benign thyroid tissue originally suspected to be a supraclavicular lymph node harboring metastatic tumor (Figure 1A). The discovery of ectopic thyroid in this patient’s case was not anticipated which raised questions about tissue characteristics, underlying etiology for FDG activity, management and follow-up.
As mentioned previously, biopsies were taken twice to confirm that the correct biopsy site was targeted. Pathological specimens were collected via ultrasound guided fine needle aspiration (Figure 2C) and ultrasound/CT-guided core biopsy (Figure 4). Discovering benign thyroid tissue in both core biopsy specimens prompted the question of whether the investigated lesion represented isolated tissue or lymph node inclusions. Several studies have demonstrated discovery of thyroid tissue in cervical lymph nodes. Triantafyllou et al. discusses how these thyroid inclusions are managed based on the histology, morphology and presence of calcifications (8). In our patient, as shown in Figure 5, there is no evidence of lymphoid tissues within the biopsy sample, thereby favoring a diagnosis of isolated ectopic thyroid over thyroid inclusions.
Besides atypical location within the supraclavicular fossa, another peculiar aspect of this case was FDG enhancement. As demonstrated in our case, FDG-PET-CT scan is commonly used in the setting of cancer staging (9). In normal thyroid tissue, FDG accumulation is reported to be generally low or absent (10). Our patient had undetectable FDG activity within his native thyroid gland but mild uptake in the focus representing ectopic thyroid tissue. Studies have shown that an increased FDG uptake has been detected in some thyroid incidentalomas, however these represent a minority of cases. Etiologies such as malignancy, inflammation and infection are more frequently associated with increased FDG activity (11,12).
While sonography is the gold standard imaging modality in evaluating thyroid lesions, as presented in this case, PET-CT scan can incidentally detect some thyroid pathologies. Thyroid lesions can appear as focal or diffuse uptake on PET scan (13). Diffuse uptake typically signifies thyroiditis or Graves disease, while focal uptake mainly represents benign or malignant nodules (12). Increased focal uptake of FDG in thyroid gland has 1–2% of prevalence for malignancy, mostly comprised of papillary carcinoma (10). Some proposed criteria guiding clinical decision to biopsy a FDG avid thyroid lesion have included palpable thyroid nodule on physical exam and focal PET radiotracer uptake (14).
SUVmax is reported as 3.4 in the present case. SUVmax is a maximum standardized value that measures the amount of FDG uptake and hypermetabolic activity (9). Interestingly, multiple studies have shown no clear correlation between the value of SUVmax for thyroid lesions and their malignant potential (12,13). Similarly, autoimmune entities such as lymphocytic thyroiditis have failed to demonstrate a strong correlation with SUVmax (10). Therefore, the cutoff for SUVmax cannot be utilized as a reliable factor for distinguishing FDG avid thyroid lesions.
Reported incidence of FDG uptake on thyroid gland ranges from 0.2–8.9%, most literature reporting 2–3% (12,13). It is unclear of an exact prevalence of malignancy on thyroid lesions detected by PET scan. Some studies have reported prevalence of cancer from FDG positive lesions on thyroid gland to be anywhere from 8% to 64% (13). Although there has been data for FDG activity reported in the thyroid gland, no data is available on the occurrence of FDG positive ectopic or accessory thyroid that are benign.
This case is unique as we present an extremely rare occurrence of FDG avid benign ectopic thyroid incidentally discovered on PET-CT during staging of esophageal adenocarcinoma. Although the FDG-active focus indicates a benign thyroid lesion, it leaves us with the question on what the appropriate follow-up would be for this particular patient. The etiology of increased FDG uptake of the ectopic thyroid tissue in this patient is unclear. From our knowledge, there are no formal recommendations on monitoring benign thyroid lesions with FDG avidity. We propose that further studies are needed to better understand the link between FDG activity and thyroid lesions as well as to identify appropriate follow-up recommendations for FDG avid thyroid lesions.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://aot.amegroups.com/article/view/10.21037/aot-21-24/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aot.amegroups.com/article/view/10.21037/aot-21-24/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lianos G, Bali C, Tatsis V, et al. Ectopic thyroid carcinoma. Case report. G Chir 2013;34:114-6. [PubMed]
- Allen E, Fingeret A. Anatomy, head and neck, thyroid. Treasure Island (FL): StatPearls Publishing, 2021.
- Richards PS, Ahuja AT, King AD. Clinics in diagnostic imaging (101): multinodular accessory thyroid tissue. Singapore Med J 2004;45:542-6. [PubMed]
- Adelchi C, Mara P, Melissa L, et al. Ectopic thyroid tissue in the head and neck: a case series. BMC Res Notes 2014;7:790. [Crossref] [PubMed]
- Soscia A, Guerra G, Cinelli MP, et al. Parapharyngeal ectopic thyroid: the possible persistence of the lateral thyroid anlage. Clinical case report. Surg Radiol Anat 2004;26:338-43. [Crossref] [PubMed]
- Tachimori Y, Ozawa S, Numasaki H, et al. Supraclavicular node metastasis from thoracic esophageal carcinoma: a surgical series from a Japanese multi-institutional nationwide registry of esophageal cancer. J Thorac Cardiovasc Surg 2014;148:1224-9. [Crossref] [PubMed]
- Choi JY, Kim JH. A case of an ectopic thyroid gland at the lateral neck masquerading as a metastatic papillary thyroid carcinoma. J Korean Med Sci 2008;23:548-50. [Crossref] [PubMed]
- Triantafyllou A, Williams MD, Angelos P, et al. Incidental findings of thyroid tissue in cervical lymph nodes: old controversy not yet resolved? Eur Arch Otorhinolaryngol 2016;273:2867-75. [Crossref] [PubMed]
- Brindle R, Mullan D, Yap BK, et al. Thyroid incidentalomas discovered on positron emission tomography CT scanning - malignancy rate and significance of standardised uptake values. Eur J Surg Oncol 2014;40:1528-32. [Crossref] [PubMed]
- Karantanis D, Bogsrud TV, Wiseman GA, et al. Clinical significance of diffusely increased 18F-FDG uptake in the thyroid gland. J Nucl Med 2007;48:896-901. [Crossref] [PubMed]
- Bakhshayesh Karam M, Doroudinia A, Joukar F, et al. Hypermetabolic thyroid incidentaloma on positron emission tomography: review of laboratory, radiologic, and pathologic characteristics. J Thyroid Res 2017;2017:7176934. [Crossref] [PubMed]
- Jamsek J, Zagar I, Gaberscek S, et al. Thyroid lesions incidentally detected by (18)F-FDG PET-CT - a two centre retrospective study. Radiol Oncol 2015;49:121-7. [Crossref] [PubMed]
- Bertagna F, Treglia G, Piccardo A, et al. Diagnostic and clinical significance of F-18-FDG-PET/CT thyroid incidentalomas. J Clin Endocrinol Metab 2012;97:3866-75. [Crossref] [PubMed]
- Are C, Hsu JF, Schoder H, et al. FDG-PET detected thyroid incidentalomas: need for further investigation? Ann Surg Oncol 2007;14:239-47. [Crossref] [PubMed]
Cite this article as: Htoo STY, Beaujean SJ, Mahmood Y, Alfonso F. Incidental diagnosis of ectopic thyroid in the work-up of metastatic esophageal cancer: a case report. Ann Thyroid 2022;7:3.


