
SARS-CoV-2 infection in patients with thyroid disease: a cross-sectional study
The SARS-CoV-2 virus has significantly impacted certain susceptible populations, leading to higher rates of morbidity and mortality, and poorer outcomes for various comorbidities (1). The main risk factors for severe infection and worse disease outcomes include the presence of multiple comorbidities (cardiovascular disease, hypertension, diabetes, and chronic respiratory disease), male gender, and older age (1). The virus is known to utilize the angiotensin-2-converting enzyme (ACE2) and transmembrane protease serine 2 (TMPRSS2) to gain entry into type II pneumocytes in human lungs (2). Interestingly, studies have noted higher levels of ACE2 and TMPRSS2 expression in the thyroid gland (3). It was recently proposed that cleavage of the SARS-CoV-2 spike protein by the furin enzyme is key to this process (4). Thyroid hormone (T3) may interfere with furin expression in the lungs hindering SARS-CoV-2 infectivity (4). However, T3 is also an important pro-inflammatory regulator in immune response during infections (4). As such, we conducted an epidemiological study to evaluate the correlation between thyroid disease and COVID-19 infection rates and severity.
This cross-sectional study used the University of California COVID Research Data Set (UC CORDS) (5), a HIPAA-limited database of medical records of patients tested for COVID-19, to collect thyroid treatment independent of hyper- or hypothyroid diagnosis; including demographics, hospitalizations within 4 weeks (+/− 2 weeks) of COVID-19 testing, and fatalities. COVID-19 patients were identified as having hyper- or hypothyroidism as a comorbidity when the medical history in the medical record mentioned either “hypothyroidism” (ICD-10 code E01.0, E03.1, E03.2, E03.9, E89.0, E06.3) or “hyperthyroidism” (ICD-10 code E05.30, E05.00, P72.1, E05.21, E05.20). These diagnoses were made from primary care providers, endocrinologists, and/or hospital-based medicine teams. Chi-squared tests were used for statistical analysis.
A total of 176,118 patients had COVID-19 tests between March and August 2020, with a 3.87% positive test rate (Table 1). A total of 1,504 hyperthyroid patients tested for COVID-19 had a 3.39% (n=51) infection rate, with no significant difference compared to those without hyperthyroidism (P=0.3300). This observation remained true when analyzing hyperthyroid men and women separately (P=0.4922, P=0.1971, respectively). Hospitalization rates were similar for patients with hyperthyroidism compared to those without (P=0.4652), and there were no difference in fatalities after positive COVID-19 test (P=0.6590).
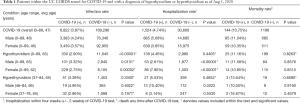
Full table
A total of 11,375 hypothyroid patients were tested for COVID-19, with a significantly lower infection rate (2.9%, n=330) compared to those without hypothyroidism (P<0.00001), which held true when separately analyzing hypothyroid men (3.32%, P=0.0101) and women (2.75%, P=0.00002). Furthermore, there was no significant difference in hospitalization rate (P=0.4405). However, when analyzing genders separately, hypothyroid men (2.61%, P<0.00001) had a significantly lower rate of hospitalization, while hypothyroid women (7.9%, P<0.00001) had an increased rate (Table 1). There were no differences in fatalities after testing positive for COVID-19 for hypothyroid patients compared to those without (P=0.8263).
In this UC CORDS dataset, both hyper- and hypothyroid patients did not have increased risk of COVID-19 infection, hospitalizations, or fatalities. Our findings suggest epidemiologic evidence of an association between hypothyroidism and reduced SARS-CoV-2 infectivity. Although we hypothesized that T3 is associated with SARS-CoV-2 infectivity through furin expression, our study showed a lower rate of infection for hypothyroid patients. This may be explained by lung tissue T3 activation through type 2 iodothyronine deiodinase (6) likely influencing inflammation, rather than being furin dependent. Also, inhaled liothyronine can inhibit lung fibrosis in rats, and there are currently clinical trials for liothyronine as treatment for acute respiratory distress syndrome, including patients with COVID-19 (7). This study was a retrospective study using data collected from the UC CORDS database of ambulatory and hospitalized COVID-19 patients. A limitation of this study is that our study population consisted solely of patients within a California-based population; therefore, limiting the generalizability of our results. Furthermore, we were unable to collect data for covariates, comorbidities, or whether patients were on thyroid hormone replacement therapy. Other study limitations include use of deidentified, tertiary center data, lack of clinical details, and rapidly changing testing criteria and availability. Future research to understand the mechanisms underlying enhanced COVID-19 susceptibility and disease severity for thyroid dysfunction will be fundamental to developing new therapies for populations at risk through large scale clinical trials.
Acknowledgements
Funding: This work was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health [UL1 TR001414].
Footnote
Provenance and Peer Review: This article was an unsolicited submission to the journal. The article did not undergo external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aot-21-8). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 2020;323:1239-42. [Crossref] [PubMed]
- Li MY, Li L, Zhang Y, et al. Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues. Infect Dis Poverty 2020;9:45. [Crossref] [PubMed]
- Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020;181:271-80.e8. [Crossref] [PubMed]
- Rubingh J, van der Spek A, Fliers E, et al. The Role of Thyroid Hormone in the Innate and Adaptive Immune Response during Infection. Compr Physiol 2020;10:1277-87. [Crossref] [PubMed]
- Health UoC. University of California Health Creates Centralized Data Set To Accelerate COVID-19 Research 2020. Available online: https://www.universityofcalifornia.edu/press-room/university-california-health-creates-centralized-data-set-accelerate-covid-19-research
- Gereben B, McAninch EA, Ribeiro MO, et al. Scope and limitations of iodothyronine deiodinases in hypothyroidism. Nat Rev Endocrinol 2015;11:642-52. [Crossref] [PubMed]
- Yu G, Tzouvelekis A, Wang R, et al. Thyroid hormone inhibits lung fibrosis in mice by improving epithelial mitochondrial function. Nat Med 2018;24:39-49. [Crossref] [PubMed]
Cite this article as: Nguyen C, Yale K, Ghigi A, Zheng K, Mesinkovska NA, Wambier CG, Cadegiani FA, Goren A. SARS-CoV-2 infection in patients with thyroid disease: a cross-sectional study. Ann Thyroid 2021;6:7.


