
Lichen planopilaris and thyroid disease: systematic review and meta-analysis
Lichen planopilaris (LPP) is a follicular subtype of lichen planus that is characterized by chronic scalp inflammation and scarring, leading to scarring alopecia (1). The etiology of LPP is thought to have an autoimmune pathogenesis, however, the precise mechanisms are not known and there is currently a lack of understanding regarding associated comorbidities. A number of studies have shown a significant association between lichen planus and thyroid disease (2), although the relationship between LPP and thyroid disease is unclear (3-5). We conducted a systematic review and meta-analysis to test the association between LPP and thyroid disease.
Electronic searches were performed using Ovid Medline, PubMed, Cochrane Central Register of Controlled Trials (CCTR), Cochrane Database of Systematic Reviews (CDSR), ACP Journal Club, and Database of Abstracts of Review of Effectiveness (DARE) from their dates of inception to July 2019. Search terms included: “lichen planopilaris” or “frontal fibrosing alopecia”, combined with “hyperthyroidism”, “hypothyroidism”, “thyroid disease”, “thyroiditis”, “thyroid cancer”. Eligible studies were those which compared dyslipidemia in cases of LPP versus controls. Case reports, reviews and studies without controls were excluded. Odds ratio (OR) was calculated using random effects model, heterogeneity was assessed using the I2 statistic. Analyses were performed using Review Manager Version 5.3 (Cochrane Collaboration, Oxford, United Kingdom). Study quality was assessed using the Newcastle-Ottawa Scale.
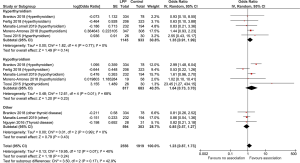
A total of 451 references were identified through electronic database searches. After applying exclusion and inclusion criteria, a final 6 studies were included for meta-analysis (Table 1). Pooled meta-analysis demonstrated no significant association between LPP and any thyroid disorders [OR 1.23; 95% confidence interval (CI), 0.87–1.73, P=0.24], with no significant heterogeneity (I2=40%, P=0.07). Subgroup analysis was performed, with no significant association found between LPP and hyperthyroidism (OR 1.35; 95% CI, 0.91–1.99; P=0.14; I2=0%) nor with hypothyroidism (OR 1.64; 95% CI, 0.73–3.70; P=0.23; I2=68%), nor with other thyroid disorders (OR 0.85; 95% CI, 0.57–1.27; P=0.43; I2=0%) (Figure 1).
Table 1
| Study | Location | Design | Cases/controls | Females % (cases/control) | Mean age in years (cases/control) | Adjustment | NOS |
|---|---|---|---|---|---|---|---|
| Brankov et al., Int J Women’s Dermatology, 2018 | USA | Case-control | 334/78 | 93.1/79.5 | 54.77/52.19 | None | 7 |
| Fertig et al., Int J Dermatology, 2018 | USA | Case-control | 206/323 | 88.35/83.28 | NA | Age, gender, ethnicity, race | 6 |
| Manatis-Lornell et al., J American Association Derm, 2019 | USA | Case-control | 232/194 | 85.3/85.1 | 61.7/65 | None | 7 |
| Moreno-Arrones et al., Clinical and Experimental Derm, 2018 | Spain | Case-control | 347/308 | 50.4/49.6 | 60/58.4 | None | 7 |
| Nguyen et al., US Endocrinology, 2016 | USA | Case-control | 28/31 | NA | NA | Age, gender, TSH | 6 |
| Toosi et al., Iranian J Derm, 2015 | Iran | Case-control | 26/30 | 69.2/70 | 52.5/54.5 | None | 6 |
NA, not reported; NOS, Newcastle Ottawa Score for study quality.
This pooled analysis of existing case-control studies to date does not support an association between LPP and any thyroid disease, hyperthyroidism or hypothyroidism. Our findings contradict those reported for lichen planus (2). As such, this suggests that there are likely differences in the nuances underlying the pathogenesis of LPP versus lichen planus. Our study has several limitations. The included studies were mostly retrospective in design, thus susceptible to selection and assessment bias. The analysed effect sizes were unadjusted, and as such susceptible to influence by confounder variables. Large database studies may have errors in coding disease parameters, and there is heterogeneity in terms of criteria for diagnosis of thyroid disorders. Prospective studies with larger numbers of patients are required to reaffirm the findings in the present study.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was a standard submission to the journal. The article did not undergo external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aot.2020.02.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tan E, Martinka M, Ball N, Shapiro J. Primary cicatricial alopecias: clinicopathology of 112 cases. J Am Acad Dermatol 2004;50:25-32. [Crossref] [PubMed]
- Li D, Li J, Li C, et al. The association of thyroid disease and oral lichen planus: a literature review and meta-analysis. Front Endocrinol (Lausanne) 2017;8:310. [Crossref] [PubMed]
- Brankov N, Conic RZ, Atanaskova-Mesinkovska N, et al. Comorbid conditions in lichen planopilaris: A retrospective data analysis of 334 patients. Int J Womens Dermatol 2018;4:180-4. [Crossref] [PubMed]
- Nguyen T, Tsai M, Grogan T, et al. Thyroid disease in alopecia areata, lichen planopilaris, and frontal fibrosing alopecia—a case control study of 144 patients. US Endocrinology 2016;12:85-6. [Crossref]
- Toossi P, Sebti A, Sarvghadi F. Thyroid diseases and lichen planopilaris: A case control study. Iran J Dermatol 2015;18:104-7.
Cite this article as: Phan K, Smith SD. Lichen planopilaris and thyroid disease: systematic review and meta-analysis. Ann Thyroid 2020;5:4.


