
The evolution and progress of anesthesia for intraoperative neuromonitoring during thyroid surgery
Introduction
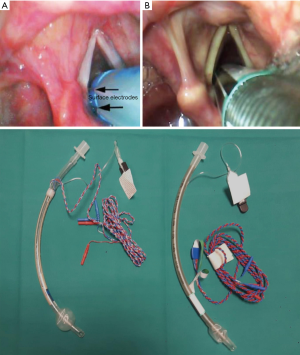
Recurrent laryngeal nerve damage during thyroid surgery was considered as an insurmountable barrier while, at present, the developments in surgical and anesthetics techniques guarantee a complete control of nerve function identifying prematurely an alteration of vocal cords function during surgical procedures (1-3). Therefore, intraoperative neuromonitoring (IONM) technique during thyroid surgery could be defined a safe procedure with some sporadic complications (4). Recently (5) we discuss about the safety of continuous IONM during thyroid surgery focusing on the importance to know extensively the implications of anaesthetics agents on sympathetic and parasympathetic tone disapproving some authors (6) that consider continuous IONM a backward step for thyroid surgery. The IONM technique in thyroid surgery started from electrostimulation applied in the surgical field with a direct visualization of muscle movements to, at present, advanced monitoring techniques through dedicated endotracheal tubes with electrodes on their surface (Figure 1).
The laryngeal nerve damage could be due to surgical blade, electrosurgical thermal lesion, direct injury during nerve isolation, nerve stretching during surgical manipulation, and perioperative edema or hematoma. Additionally anatomical variations, reoperation and history of previous neck irradiation are less common causes (7-9). Thomusch et al. (10) showed that an optimal IONM signal at the end of surgical procedure is related to normal vocal cord function in 99.6% of cases, while 30−45% of patients with postoperative vocal cord dysfunction have an intraoperative altered signal. According with these data, in the era of Evidence Base Medicine, the IONM technique is becoming the standard of care (11). The anesthesiological approach has developed through recent years according with technical evolution. The use of dedicated endotracheal tube has many implications during anesthesia induction; as well the rational use of ipnotic agents and the introduction of new drugs. Therefore clinicians must be aware of this technological development maintaining a cooperation approach with the surgeon during intraoperative nerve monitoring. In this manuscript we describe the main concerns for anesthetists during IONM technique focusing on its development during last years.
Continuous IONM (C-IONM) and intermittent IONM (I-IONM)
Two type of intraoperative nerve stimulation are described in literature: I-IONM and C-IONM. Intermittent approach consists on primary vagal stimulation to confirm correct endotracheal tube placement, to assess the absence of prior defects on vocal cord activity and confounding factors (curare, tube dislodgement, device malfunction) than an intermittent stimulation to inferior laryngeal nerve during thyroid excision. Additionally the recent dedicated endotracheal tubes permit to assess the superior laryngeal nerve as an adjunct to maintain a complete integrity of laryngeal innervation. The continuous intraoperative stimulation, instead, provides continuous vagal nerve stimulation during surgical procedure. The continuous approach was developed to transform intermittent information (nerve integrity) into continuous information (12). Well known are the risk connected to this technique due to opening of the carotid sheath, circumferential dissection of the vagal nerve, difficulties of implanting electrodes and the potential side effects of vagal nerve stimulation (13,14). For this reasons some authors criticize this approach, point out the possible problems occurring with this technique (6). For the anesthesiologists is mandatory to well know this procedure.
During general anaesthesia the balance of autonomic nervous system is transformed. The continuous propofol perfusion reduces blood pressure and parasympathetic tone in direct proportion to the depth of anesthesia, while the halogenated drugs have minor effects on the parasympathetic tone (15). The neuromonitoring devices, such as BiSpectral Index, are essential to avoid haemodynamic instability due to inappropriate depth of anaesthesia during surgical manipulation and to discriminate from further causes. The use of continuous supramaximal currents ranged from 0.5 to 5 mA, pulse width 200 s, pulse rate 2 s does not reveal any haemodynamic instability in terms of heart rate and pressure variability despite an incremental tone of vagal nerve (16). This data points out the importance to maintain a proactive anesthesiological intraoperative approach in accordance with patient comorbidities. The main molecules used for general anesthesia in this specific surgical setting have hemodynamic effects not C-IONM related. Likewise it‘s important to monitor the anaesthesia depth to avoid an alteration, pharmacological mediated, of the autonomic nervous system.
Additionally we would emphasize the anatomical implication (17) during IONM with continuous vagal stimulation. While the right vagus nerve is closely associated with the cardiac atrium, the left vagus nerve is associated with the ventricles. The ventricles are less densely innervated (vagal innervation) than the atriums, therefore the response of continuous right vagal nerve stimulation could provoke some undesired rhythm disturbances determined by efferent right vagal fibres. The main advantage of continuous versus intermittent stimulation is that it allows continuous monitoring without further intervention of the surgeon or the assistant, it offers a good visibility during thyroid surgery avoiding accidentally recurrent laryngeal injury.
The anesthesia evolution
The pillar of anaesthesia during IONM technique in thyroid surgery is to guarantee the best signal during surgical procedures, avoiding all confounding factors. The main challenge for the anesthetists is to proceed with correct positioning of the dedicated endotracheal tubes with electrodes close to vocal cords. In literature it is described an incidence of moderate or severe laryngeal damage approximatively below 10% during thyroid surgery (18). The use of neuromuscular blocking agents (NMBAs) facilitates the visualization of the vocal cords during laryngoscopy simplifying the tracheal tube insertion. The technical specifications of endotracheal tubes for IONM point out that the use of NMBA alters the signals. However, in our practice, with literature support, we use NMBA during induction to ensure a correct insertion of dedicated endotracheal tube (19). The faster curare clearance due to the wide vascularization of upper airway and the broad presence of neuromuscular junction into larynx guarantee an adequate signal at the start of surgical procedure. It’s recommendable to use lower dosage of curare with some adjuvants such as intraoral lidocaine. Lidocaine is a short acting local anaesthetic and its use during laryngoscopy permits to reduce the sensitive responses to tracheal intubation. The topical lidocaine is contraindicated by ETTs (Endotracheal tubes) producers but its use doesn’t alter NIM intraoperative signal (20). During emergence from anaesthesia is important to avoid excessive cough and immediate pain; lidocaine with its biphasic peak serum level (21) guarantees a good postoperative pain relief and a down regulation of cough reflex. Recently (22), Sugammadex, the reversal of non-depolarizing blocking agents (Rocuronium and Vecuronium) has been adopted in a recovery protocol to restore muscular function after NMBAs administration in thyroid surgery. This drug restores respiratory activity during unanticipated difficult airways and it is considered an optimal aid during general anesthesia recovery. During thyroid surgery with IONM technique, the anesthetists have to contemplate its use to optimize the signals after NMBAs use.
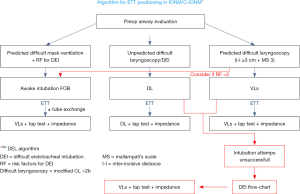
The anticipated or unanticipated difficult airway have to be managed according with existing guidelines (23). To reduce the failure during tracheal intubation with dedicated endotracheal tubes, we have to focus on new devices that help during this manoeuvre. The videolaryngoscopy is an optimal instrument to visualize vocal cords and subsequently to arrange the electrodes closer to vocal cords (24,25). As described, the videolaryngoscopy facilitates the intubation at first attempt and it is an aid in high degree of Cormack-Lehane scale. In addition, all the clinicians involved in patient care (surgeon and nurse staff) could appreciate a correct tube placement into the operating room video (Figure 1). In our centre we developed a simplified algorithm to facilitate the decision making process for airway management (Figure 2). In according with recent guidelines, we encourage the use of video assisted intubation devices in case of predicted difficult airway. The anaesthesia maintenance during surgery is controversial for IONM procedures. The better anaesthetic technique is tailored on patient comorbidities but several studies have shown that halogenated agents and nitrous oxide depress IONM signals than total intravenous anaesthesia (TIVA) (26). Inhaled anesthesia isn’t contraindicated during thyroid surgery with IONM but the use of TIVA increases the muscle relaxation due to propofol pharmacodynamics guarantying a better intraoperative signal. The remifentanil continuous infusion addicted to propofol reduces cough reflexes and guarantees an optimal intraoperative pain management. In addition, TIVA use reduces postoperative nausea and vomiting, anesthesia side effects that could influence the surgical success in term of haematoma onset.
Medical legal aspects
The IONM technique during thyroid surgery has increased during these years thanks to implementation of clinician knowledge and costs reduction. Surgical consent is a medical act where the patient has to be aware about all surgical alternatives and all intraoperative strategies, therefore IONM technique with “pro” and “con” is an available option with a consistent literature support. The anesthetists during consent achievement have to explain to the patients all the risk related to IONM technique and have to focus on clinical preoperative signs of alteration in nerve integrity. All preventable complications related to intubation and nerve stimulation could be assessed and discussed with the patient. The clinicians have to proceed with a shared decision making process where the patients manifest their choice according with the clinical practice and the evidence based medicine. Therefore the clinicians have to demonstrate the importance of IONM technique according with scientific evidence pointing out the benefits but also the related complications. According with recent manuscript (27) we agree that there are not guaranties to preserve nerve function with IONM technique but we can observe a reduction of nerve damage, which is currently below 2%.
Conclusions
Thyroid surgery evolved through recent years and the use of IONM technique represents the main development to identify nerves and to assess the real time intraoperative nerve integrity. The IONM in thyroid surgery from first manuscript in 1969 (28) to recent literature has developed according with technical improvement and anesthesia challenges are due to maintain an optimal standard of care avoiding any disturbances during monitoring process. The anesthesiologists, involved into thyroid surgery, have to be aware about correct endotracheal tube position without any improper use of anaesthetic drugs. In clinical practice, we recommend emphasizing the preoperative assessment of the patients focusing on airway management and, additionally, about preoperative comorbidities, such as atrioventricular block, that could be affected by IONM technique. In conclusion, we found strong evidence to support IONM technique in experienced operating teams within appropriate setting.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Marcin Barczyński, Hui Sun, and Xiaoli Liu) for the series “The Protection and Monitoring of Superior and Recurrent Laryngeal Nerve in Thyroid and Parathyroid Surgery” published in Annals of Thyroid. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aot.2018.11.03). The series “The Protection and Monitoring of Superior and Recurrent Laryngeal Nerve in Thyroid and Parathyroid Surgery” was commissioned by the editorial office without any funding or sponsorship. Gianlorenzo Dionigi served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Annals of Thyroid from Mar 2017 to Feb 2019. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the manuscript and ensure that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Périé S, Ait-Mansour A, Devos M, et al. Value of recurrent laryngeal nerve monitoring in the operative strategy during total thyroidectomy and parathyroidectomy. Eur Ann Otorhinolaryngol Head Neck Dis 2013;130:131-6. [Crossref] [PubMed]
- Hermann M, Alk G, Roka R, et al. Laryngeal recurrent nerve injury in surgery for benign thyroid diseases: effect of nerve dissection and impact of individual surgeon in more than 27,000 nerves at risk. Ann Surg 2002;235:261-8. [Crossref] [PubMed]
- Dralle H, Sekulla C, Lorenz K, et al. Intraoperative monitoring of the recurrent laryngeal nerve in thyroid surgery. World J Surg 2008;32:1358-66. [Crossref] [PubMed]
- Chen P, Liang F, Li L, et al. Complications and adverse effects associated with intraoperative nerve monitoring during thyroid surgery under general anesthesia. Cell Biochem Biophys 2015;71:1029-33. [Crossref] [PubMed]
- Bacuzzi A, Dralle H, Randolph GW, et al. Safety of Continuous Intraoperative Neuromonitoring (C-IONM) in Thyroid Surgery. World J Surg 2016;40:768-9. [Crossref] [PubMed]
- Terris DJ, Chaung K, Duke WS. Continuous vagal nerve monitoring is dangerous and should not routinely be done during thyroid surgery. World J Surg 2015;39:2471-6. [Crossref] [PubMed]
- Calò PG, Pisano G, Medas F, et al. Intraoperative recurrent laryngeal nerve monitoring in thyroid surgery: is it really useful? Clin Ter 2013;164:e193-8. [PubMed]
- Calò PG, Pisano G, Medas F, et al. Risk factors in reoperative thyroid surgery for recurrent goitre. Our experience. G Chir 2012;33:335-8. [PubMed]
- Loch-Wilkinson TJ, Stalberg PL, Sidhu SB, et al. Nerve stimulation in thyroid surgery: is it really useful? ANZ J Surg 2007;77:377-80. [Crossref] [PubMed]
- Thomusch O, Sekulla C, Machens A, et al. Validity of intra-operative neuromonitoring signals in thyroid surgery. Langenbecks Arch Surg 2004;389:499-503. [Crossref] [PubMed]
- Dionigi G, Chai JY, Freni F, et al. The Consistency of Intraoperative Neural Monitoring in Thyroid Surgery. J Endocr Surg 2018;18:e15. [Crossref]
- Schneider R, Randolph GW, Sekulla C, et al. Continuous intraoperative vagus nerve stimulation for identification of imminent recurrent laryngeal nerve injury. Head Neck 2013;35:1591-8. [Crossref] [PubMed]
- Dionigi G, Donatini G, Boni L, et al. Continuous monitoring of the recurrent laryngeal nerve in thyroid surgery: a critical appraisal. Int J Surg 2013;11:S44e6.
- Wu CW, Dionigi G, Chen HC, et al. Vagal nerve stimulation without dissecting the carotid sheath during intraoperative neuromonitoring of the recurrent laryngeal nerve in thyroid surgery. Head Neck 2013;35:1443e7.
- Kanaya N, Hirata N, Kurosawa S, et al. Differential effects of propofol and sevoflurane on heart rate variability. Anesthesiology 2003;98:34-40. [Crossref] [PubMed]
- Ulmer C, Friedrich C, Kohler A, et al. Impact of continuous intraoperative neuromonitoring on autonomic nervous system during thyroid surgery. Head Neck 2011;33:976-84. [Crossref] [PubMed]
- Janes RD, Brandys JC, Hopkins DA, et al. Anatomy of human extrinsic cardiac nerves and ganglia. Am J Cardiol 1986;57:299-309. [Crossref] [PubMed]
- Birkholz T, Irouschek A, Saalfrank-Schardt C, et al. Laryngeal morbidity after intubation with or without neuromuscalr block in thyroid surgery using recurrent laryngeal nerve monitoring. Auris Nasus Larynx 2012;39:288-93. [Crossref] [PubMed]
- Mencke T, Echternach M, Kleinshmidt S, et al. Lryngeal morbidity and quality of tracheal intubation Anethesiology 2003;98:1049-56.
- Pachuski J, Vaida S, Donahue K, et al. Effect of laryngotracheal topical anesthesia on recurrent laryngeal nerve monitoring during thyroid surgery. J Clin Anesth 2016;29:10-3. [Crossref] [PubMed]
- Prengel AW, Lindner KH, Hahnel JH, et al. Pharmacokinetics and technique of endotracheal and deep endobronchial lidocaine administration. Anesth Analg 1993;77:985-9. [Crossref] [PubMed]
- Lu IC, Wu CW, Chang PY, et al. Reversal of rocuronium-induced neuromuscular blockade by sugammadex allows for optimization of neural monitoring of the recurrent laryngeal nerve. Laryngoscope 2016;126:1014-9. [Crossref] [PubMed]
- Frerk C, Mitchell VS, McNarry AF, et al. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth 2015;115:827-48. [Crossref] [PubMed]
- Kanotra SP, Kuriloff DB, Lesser J, et al. GlideScope-assisted nerve integrity monitoring tube placement for intra-operative recurrent laryngeal nerve monitoring. J Laryngol Otol 2012;126:1271-3. [Crossref] [PubMed]
- Berkow L, Dackiw AP, Tufano RP. Use of the Glidescope for placement of a recurrent laryngeal nerve monitoring endotracheal tube. J Clin Anesth 2011;23:81-3. [Crossref] [PubMed]
- Deiner S. Highlights of anesthetic consideration for intraoperative neuromonitoring. Semin Cardiothorac Vasc Anesth 2010;14:51-3. [Crossref] [PubMed]
- Demontis R, Pittau MR, Maturo A, et al. Medico legal aspects on neuromonitoring in thyroid surgery: informed consent on malpractice claims. G Chir 2017;38:149-54. [Crossref] [PubMed]
- Flisberg K, Lindholm T. Electrical stimulation of the huan recurrent laryngeal nerve during thyroid operation. Acta Otolaryngol Suppl 1969;263:63-7. [PubMed]
Cite this article as: Guzzetti L, Dionigi G, Cuffari S, Bacuzzi A. The evolution and progress of anesthesia for intraoperative neuromonitoring during thyroid surgery. Ann Thyroid 2018;3:33.


