
Spontaneous thyroid hemorrhage management: a case report
Highlight box
Key findings
• In case of bleeding into the thyroid cyst aspiration or draining to decompress the airways are needed. In case of continuous bleeding a patient may require hemithyroidectomy.
What is known and what is new?
• Thyroid hemorrhage is a rare event and reported in incidental case reports.
What is the implication, and what should be changed?
• If a patient has dyspnea, increase in the thyroid mass volume, hemodynamic instability an emergency surgical intervention is required.
Introduction
Thyroid nodules are a common clinical problem. Epidemiological studies have shown that the prevalence of palpable thyroid nodules is approximately 5% in women and 1% in men living in iodine-sufficient parts of the world (1,2). At the same time, ultrasonography (USG) can detect thyroid nodules in 19–68% of patients, more often in women and elderly patients (3-6). The clinical importance of thyroid nodules is associated with the need to exclude thyroid cancer, which occurs in 7–15% of cases depending on age, gender, family history and other factors (7-9). Some of these nodules are purely or predominantly cystic and require only observation (10). One of the rare complications is the thyroid cyst hemorrhage. Spontaneous hemorrhage into the thyroid gland is a rare phenomenon that occurs in both multinodular and single-nodular goiters. The possible cause may be trauma or ulceration of a large feeding vessel. Although the clinical course is mostly favorable, this is a medical emergency requiring careful evaluation because, in rare cases, active bleeding can cause airway obstruction requiring intubation and surgery (6). The true incidence of spontaneous thyroid hemorrhage into the cyst or parenchyma is not known as there are only incidental case reports in the literature.
This clinical observation provides an example of spontaneous hemorrhage into a thyroid cyst with airway compression and dyspnea. We present this case in accordance with the CARE reporting checklist (available at https://aot.amegroups.com/article/view/10.21037/aot-23-34/rc).
Case presentation
A 42-year-old female first began to notice pain in the neck and a nodule on the right since September 1, 2022. On September 7, 2022, she noted acute worsening of her neck pain, increase in the nodule size and she was urgently hospitalized. During neck examination there was a mass on the right, with the size of 6 cm × 8 cm (Figure 1), painful on palpation (visual analog scale score 4/10). There were no signs of hyperthermia and hyperemia. She had a mild anemia in her laboratory tests (Hb 112 g/L). Neck USG revealed a rounded thick-walled with heterogeneous echogenicity with circulating blood flow in the Doppler mode, 84 mm × 48 mm in size. We performed a USG-guided puncture and 40 mL of hemorrhagic content was obtained. The patient did not report any trauma, medication or chronic conditions. She was closely monitored but due to the rapid increase in the cyst volume, pain sharpening, compression of surrounding tissues and dyspnea [Medical Research Council (MRC) dyspnea scale 3], we decided to perform right-sided hemithyroidectomy. Cefotaxime 1 g was administered intravenously 30 minutes before surgery as an antibiotic prophylaxis. Surgery was performed under general anesthesia. A collar incision was made on the anterior surface of the neck without crossing the pretracheal muscles. The thyroid gland was exposed, the left lobe, the isthmus and the right lobe had dimensions of 4.0 cm × 2.0 cm × 1.5 cm, 1.5 cm × 1.0 cm × 0.5 cm and 3.5 cm × 2.5 cm × 3.0 cm respectively. The left lobe contained a volumetric mass of a soft, elastic consistency, 8.0 cm × 4.0 cm × 3.0 cm in size. The trachea was displaced to the left by the mass. Using bipolar coagulation mode, the thyroid cyst was removed (Figure 2). After further mobilization of the right lobe heterogeneous nodes up to 1 cm in diameter were seen. Hemithyroidectomy was performed with the right recurrent laryngeal nerve visualization. An active suction drain was installed in the thyroid bed. The wound was sutured layer by layer with the use of cosmetic stitches. In the postoperative period the patient received symptomatic treatment with non-steroidal anti-inflammatory drugs (NSAIDs) (ketorolac 30 mg IV) and his serum calcium level was within normal reference range during monitoring. On day 3 after the operation, the drain was removed and control USG was performed, which showed only signs of soft tissue edema in the area of intervention, no fluid accumulation was detected. The patient was discharged from the hospital on the same day.
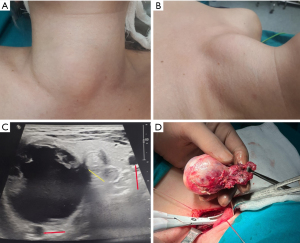
Pathological examination of the right lobe of the thyroid gland identified foci of moderate chronic thyroiditis without signs of active inflammation. Also a picture of macrofollicular growth pattern in a colloid nodular goiter with cystic transformation was detected. There were signs of edematous stroma and the periphery of the right lobe of the thyroid gland was represented by a hyalinized stroma, compressed follicles similar to a pseudoadenoma, lymphocytic and histiocytic infiltration. Hence, the right lobe mass was a colloid goiter with cystic dystrophy, intraparenchymal hemorrhages, focal lymphocytic nonspecific thyroiditis with areas of sclerosis and follicular adenomas.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Integration of thyroid imaging techniques into everyday practice has led to an increase in the number of diagnosed of thyroid nodules (3). Many of these nodules are purely cystic or predominantly cystic (≥60% of cystic component). Cystic nodules are considered to have a mild risk of malignancy (pure cysts are less than 1%, partially cystic nodules with no suspicious features are less than 3%, partially cystic nodules with eccentric solid areas with minor suspicious features are 5–10% likely to be malignant. Therefore, they are usually observed and do not require active treatment. However, in some cases cystic thyroid nodules require observation and treatment, such as rapid growth, cosmetic defects, or local compression symptoms (neck pain, dysphagia, dyspnea, and cough) (10). In rare cases thyroid nodules can lead to such complication as intraparenchymal hemorrhage. Most often it occurs due to trauma, unlike in the presented case. However, it can also occur in case of abundant blood supply of the nodule, supplying vessels ulceration, arteriovenous shunts formationand the presence of a spongy mass (11). Another risk factor of spontaneous hemorrhage is deviations in blood clotting, overdose of antiplatelet agents and anticoagulants. Traumatic factors are the thyroid gland microwave ablation (MVA) and cyst cavity puncture (12).
The currently available treatment options include ultrasound-guided cyst puncture, ablation or surgical removal (13). These procedures are not performed often as thyroid cysts are benign and usually asymptomatic. The recurrence rate after puncture and aspiration is high and occurs in 60–90% of patients (14). Surgical removal is a definitive treatment but may be associated with more complications (15). The complication rate of MVA is much lower than that of surgical removal. However, there is still a risk of nodule rupture after ablation. Shin et al. reported that the mean preoperative nodule volume was greater than 17.1 mL in 6 cases of nodule rupture after ablation (16). In our case, a relatively large volume (more than 40 mL) and abundant blood flow in thyroid nodules were high risk factors for the rupture of the nodule and was also a contraindication for ablation. A total of 30 cases of nodule rupture after ablation have been described in 6 studies with an incidence ranging from 0.2% to 2.4% (17). Spontaneous rupture with bleeding into thyroid cysts, which required surgical intervention, is described only in single observations.
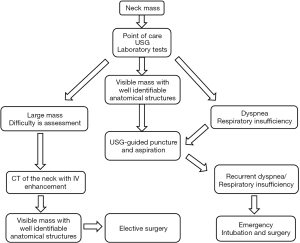
Neck masses usually are evaluated as congenital anomalies, inflammatory or infectious conditions and tumors (18). The thyroid gland tumors are common but usually do not present as an acute condition. A neck mass that appears spontaneously and is increasing in size might be because of bleeding and should undergo evaluation in emergency settings. The management of this group of patients depends primarily on the amount of bleeding and airway patency. The authors present an algorithm for the management of this situation based on the presented case report, literature and clinical experience (Figure 2). In order to assess the degree of compression of the surrounding tissues, the most optimal method is point-of-care USG. Decompression can be performed by USG-guided puncture or by inserting a drain into the cavity. Cystic component will help determine the further tactics of treatment and differential diagnosis with an abscess. In most cases, bleeding stops with the use of conservative therapy. The patient should undergo complete blood count, coagulation panel and thyroid hormones level [T3, T4, thyroid-stimulating hormone (TSH)] evaluation. The latter should be performed as thyroid trauma which can lead to subacute, acute thyroiditis and in severe cases to thyroid storm. In case if the patients receive antiplatelet therapy or anticoagulants they must be stopped and, if possible, reversed. Intravenous (IV) contrast-enhanced computed tomography (CT) should be performed in stable patients as it allows to determine extravasation and provides more data about the head and neck region. Appearance or increase of dyspnea, a mass volume increase, hemodynamic instability call for an emergency surgical intervention. Conservative treatment should include antibiotic therapy to prevent abscess formation and anti-inflammatory therapy to reduce swelling. If patient’s medical state worsens, one should undergo emergency intubation for airways protection and surgical treatment, which most often includes hemorrhage control and hemithyroidectomy (Figure 2).
Conclusions
Spontaneous hemorrhage into the thyroid gland is a rare phenomenon that occurs when a feeding vessel rupture or erosion of a thyroid mass occurs. Mostly, it has good prognosis and requires conservative therapy and observation. Rarely, active bleeding can cause airway obstruction, requiring urgent intubation and emergency surgery.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://aot.amegroups.com/article/view/10.21037/aot-23-34/rc
Peer Review File: Available at https://aot.amegroups.com/article/view/10.21037/aot-23-34/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aot.amegroups.com/article/view/10.21037/aot-23-34/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work and ensure that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Vander JB, Gaston EA, Dawber TR. The significance of nontoxic thyroid nodules. Final report of a 15-year study of the incidence of thyroid malignancy. Ann Intern Med 1968;69:537-40. [Crossref] [PubMed]
- Tunbridge WM, Evered DC, Hall R, et al. The spectrum of thyroid disease in a community: the Whickham survey. Clin Endocrinol (Oxf) 1977;7:481-93. [Crossref] [PubMed]
- Durante C, Grani G, Lamartina L, et al. The Diagnosis and Management of Thyroid Nodules: A Review. JAMA 2018;319:914-24. [Crossref] [PubMed]
- Tan GH, Gharib H. Thyroid incidentalomas: management approaches to nonpalpable nodules discovered incidentally on thyroid imaging. Ann Intern Med 1997;126:226-31. [Crossref] [PubMed]
- Guth S, Theune U, Aberle J, et al. Very high prevalence of thyroid nodules detected by high frequency (13 MHz) ultrasound examination. Eur J Clin Invest 2009;39:699-706. [Crossref] [PubMed]
- Covino M, Princi P, De Luca G, et al. Spontaneous thyroid nodule hemorrhage in the emergency department. Endocr Pract 2020;26:192-6. [Crossref] [PubMed]
- Hegedüs L. Clinical practice. The thyroid nodule. N Engl J Med 2004;351:1764-71. [Crossref] [PubMed]
- Mandel SJ A. 64-year-old woman with a thyroid nodule. JAMA 2004;292:2632-42. [Crossref] [PubMed]
- Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016;26:1-133. [Crossref] [PubMed]
- Iñiguez-Ariza NM, Lee RA, Singh-Ospina NM, et al. Ethanol Ablation for the Treatment of Cystic and Predominantly Cystic Thyroid Nodules. Mayo Clin Proc 2018;93:1009-17. [Crossref] [PubMed]
- Yang H, Zhao S, Zhang Z, et al. The associated factors for spontaneous intranodular hemorrhage of partially cystic thyroid nodules: A retrospective study of 101 thyroid nodules. Medicine (Baltimore) 2020;99:e23846. [Crossref] [PubMed]
- Gunasekaran K, Rudd KM, Murthi S, et al. Spontaneous Thyroid Hemorrhage on Chronic Anticoagulation Therapy. Clin Pract 2017;7:932. [Crossref] [PubMed]
- Baek JH, Ha EJ, Choi YJ, et al. Radiofrequency versus Ethanol Ablation for Treating Predominantly Cystic Thyroid Nodules: A Randomized Clinical Trial. Korean J Radiol 2015;16:1332-40. [Crossref] [PubMed]
- Castro MR, Iniguez-Ariza NM, Lee RA, et al. In Reply-Ethanol Ablation of Cystic Thyroid Nodules. Mayo Clin Proc 2019;94:171. [Crossref] [PubMed]
- Dong S, Sun L, Xu J, et al. Intracystic Hemorrhage and Its Management During Ultrasound-Guided Percutaneous Microwave Ablation for Cystic Thyroid Nodules. Front Endocrinol (Lausanne) 2020;11:477. [Crossref] [PubMed]
- Shin JH, Jung SL, Baek JH, et al. Rupture of benign thyroid tumors after radio-frequency ablation. AJNR Am J Neuroradiol 2011;32:2165-9. [Crossref] [PubMed]
- Tian P, Du W, Liu X, et al. Ultrasonographic characteristics of thyroid nodule rupture after microwave ablation: Three case reports. Medicine (Baltimore) 2021;100:e25070. [Crossref] [PubMed]
- Schwetschenau E, Kelley DJ. The adult neck mass. Am Fam Physician 2002;66:831-8. [PubMed]
Cite this article as: Dolidze DD, Bagatelia ZA, Mulaeva KA, Kolotilshchikov AA, Gogitidze NN, Bumbu A, Covantsev S. Spontaneous thyroid hemorrhage management: a case report. Ann Thyroid 2024;9:2.


