
A systematic review of trainee involvement in thyroid surgery and the impact on patient outcomes
Introduction
Surgical trainees are expected to be competent in performing operations independently by the end of their training. This often involves spending hundreds of hours performing increasingly complex operations under the close supervision of their consultants. Additionally, consultants are expected to provide training opportunities for their trainees without jeopardising clinical outcomes. In the current literature, numerous studies in the speciality of general surgery have reported that trainee involvement has no impact on clinical outcomes (1,2), while others have reported an increase in operating times (3) and complication rates (4,5).
Thyroidectomy is one of the most common endocrine surgical operations performed by ear, nose and throat (ENT) surgeons and general surgeons with an interest in endocrine surgery. There is a direct correlation between surgeon volume and its impact on clinical outcomes, with a yearly minimum of 20–25 thyroidectomies recommended to maintain low complication rates (6,7); however, a learning curve of at least 60 thyroidectomies may be required (8). With current working time restrictions, trainees may find obtaining operative experience to gain competencies in thyroidectomies difficult, yet are expected to have favourable outcomes.
Several clinical outcomes are of great importance in thyroid surgery. These outcomes include hypocalcaemia, recurrent laryngeal nerve injury, re-bleeding rates and operating times. Trainee involvement in thyroid surgery may have both positive and negative impacts on clinical outcomes. The aim of this systematic review is to assess and provide a review of the literature as it relates to trainee involvement in thyroid surgery and their impact on clinical outcomes.
Methods
Search strategy
A search strategy was developed to identify all studies involving patients undergoing thyroidectomy with trainee involvement and their impact on clinical outcomes. An electronic search of online databases (MEDLINE, Cochrane and EMBASE) was performed to include studies from 1995 to 2018. The following terms were used for the search, using Boolean operators ‘OR’ and ‘AND’: ‘thyroidectomy’, ‘hemithyroidectomy’ or ‘thyroid surgery’ combined with ‘training’, ‘trainees’, ‘residents’ or ‘residency’.
Inclusion criteria
Studies were included if they compared clinical outcomes of patients undergoing thyroid surgery by trainees versus consultants. Studies involving ENT and general surgery trainees were also included. Studies that had other operations were also included but individual data specific to thyroid surgery was extracted (see Table 1). The search was filtered to include publications involving patients over 18 years of age.
Table 1
| Author | MINORS score | Country | Type of study | Patients, n | Intervention | Outcomes reported | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Consultant operating | Trainee operating | Hypocalcaemia | Nerve injury | Re-bleeding | Operating time | |||||
| Hassan et al. | 14 | Germany | Retrospective | 111 | 42 | TT | Yes | Yes | No | No |
| Acun et al. | NA* | Turkey | Prospective | 74 | 78 | nTT | Yes | Yes | Yes | No |
| Folsom et al. | 12 | USA | Retrospective | 4,457 | 8,694 | HT | No | No | No | Yes |
| Ambe et al. | 18 | Germany | Retrospective | 147 | 61 | HT/TT | Yes | Yes | Yes | Yes |
| Gurrado et al. | 16 | Multicentre | Retrospective | 7,092 | 1,816 | TT | Yes | Yes | Yes | Yes |
| Mishra et al. | 16 | India | Retrospective | 127 | 105 | TT | Yes | Yes | Yes | No |
| Vieira et al.** | 13 | USA | Retrospective | NA | NA | T* | No | No | No | Yes |
| Emre et al. | 20 | Turkey | Prospective | 69 | 75 | TT | Yes | Yes | Yes | Yes |
| Uecker et al.** | 17 | USA | Retrospective | NA | NA | T* | No | No | No | Yes |
| Reinisch et al. | 16 | Germany | Retrospective | 112 | 112 | TT/HT/nTT | Yes | Yes | Yes | Yes |
n, number; TT, total Thyroidectomy; nTT, near total thyroidectomy; HT, hemi-thyroidectomy; T*, thyroidectomy type not indicated; NA, not available; NA*, not applicable. Studies with ** are those where data was extracted.
Exclusions
Studies that were not comparative in nature were excluded.
Study selection
After performing a search of the literature, all relevant abstracts mentioning trainee versus consultant involvement in thyroid surgery and the impact on clinical outcomes were screened by the first author. Full texts were then screened by 2 authors to ensure they met the inclusion criteria of the study and that they fulfilled the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (9).
Further studies were included after searching the references of the studies obtained from the electronic search. Any queries about suitability for inclusion were resolved by consensus.
Outcomes measured
The main outcomes of interest were hypocalcaemia rates and injury to the recurrent laryngeal nerve. Hypocalcaemia was defined as calcium below the normal reference range and/or requiring calcium supplementation. Hypocalcaemia was further divided into temporary versus permanent hypocalcaemia depending on the need for further calcium supplementation at 6 months follow up. Injury to the recurrent laryngeal nerve was defined as voice changes as a result of direct injury to the nerve and confirmed by video laryngoscopy. Nerve injury was also divided into temporary or permanent based on the persistence on voice changes at 6 months follow up.
The secondary outcomes of interest were re-bleeding rates and operating times. Re-bleeding was defined as the need for subsequent return to theatre due to significant swelling in the neck or airway compromise in the post-operative period (before discharge from hospital). Operative time was defined as the time from initial skin incision to skin closure.
Quality assessment
The quality of the methods was assessed independently by 2 authors. The MINORS criteria (Methodological index for Non-Randomized Studies) were used to assess the quality of the methods used in the included studies (10). It is a validated 12-item tool used to assess the quality of non-randomised comparative studies. Each item is scored from 0–2, giving a maximum score of 24. The MINORS score for 9 of the studies are included in Table 1. Acun et al. (11) was not assessed using the MINORS criteria as this was a randomised study.
Results
Search strategy
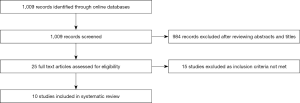
A total of 1,009 papers were identified and their titles were screened. After screening 984 were excluded. Twenty-five full texts were then assessed for eligibility of which 15 were assessed to be not eligible for inclusions. Ten studies met the eligibility criteria and were included in this review (Figure 1).
Included study characteristics
Table 1 summaries the characteristics of the 10 studies included in this review. Three studies were from Germany and United States, 2 from Turkey, 1 study was a European-multicentred and 1 study was from India. Included studies were from 1999 to 2016. Of the 10 studies, 8 were retrospective and 2 prospective. There was 1 multicentre study. There was heterogeneity in the included studies – type of operation (hemithyroidectomy, total thyroidectomy, near total thyroidectomy), population studies (Graves’s disease, diagnostic hemithyroidectomy, thyroid cancer) and reporting of outcomes measured.
Two studies were based on data from registries and examined multiple surgical operations (12,13). In these 2 studies data was extracted where available. The remaining 8 studies examined trainee involvement in thyroid surgery only. Only 4 studies examined all clinical outcomes specified in this review
Statistical analysis
Due to this heterogeneity, a meta-analysis could not be performed and a narrative systematic review was utilised instead
Outcomes
Figure 2 summarises the results of the individual studies.
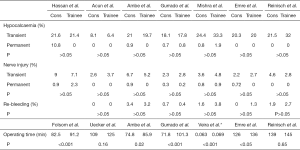
Hypocalcaemia
Seven studies assessed the impact of trainee involvement in thyroidectomies on hypocalcaemic rates (11,14,15-19). All studies reported no significant differences in temporary or permanent hypocalcaemia rates when comparing trainee versus consultant involvement in thyroidectomies.
Hassan et al. (14), Acun et al. (11), Ambe et al. (15), Gurrado et al. (16), Emre et al. (18), and Reinsch et al. (19) defined hypocalcaemia as ionised calcium below the reference range and/or symptoms of hypocalcaemia such as tingling or paraesthesia. They further subdivided hypocalcaemic rates into temporary or permanent based on an interval time period of 6 months. Mishra et al. (17), although reporting hypocalcaemia rates, did not clearly define hypocalcaemia in his methodology.
Rates of temporary hypocalcaemia for trainees ranged from 6.4–33% and permanent hypocalcaemia from 0–1.9%. Rates of temporary hypocalcaemia for consultants ranged from 8.1–24% and permanent hypocalcaemia from 0–0.8%.
Nerve injury
Seven studies assessed the impact of trainee involvement on nerve injury rates (11,14,15-19). All studies reported no significant differences in temporary or permanent nerve injury rates when comparing trainee to consultant involvement.
Six of those studies defined nerve injury based on the presence of vocal cord paresis on post-operative laryngoscopy. Mishra et al. (17), although reporting on nerve injury did not mention how this was assessed. Temporary and permanent nerve injuries were examined in the 7 included studies. Three studies (16,18,19) defined permanent nerve injury on follow up periods ranging from 3–6 months.
Rates of temporary nerve injury for trainees ranged from 2.7–7.1% and permanent injury from 0–2.3%. Rates of temporary nerve injury for consultants ranged from 2.2–9% and permanent injury from 0–0.9%.
Re-bleeding
Six studies assessed re-bleeding rates (11,15-19). Gurrado et al. (16), Emre at al. (18) and Reinisch et al. (19) clearly stated whether post-op bleeding required re-intervention or conservative management.
All 3 studies found no difference in re-bleeding rates among trainees and consultants. Re-bleeding rates requiring intervention for both trainees and consultants ranged from 0–1%.
Ambe et al. (15), Acun et al. (11) and Mishra et al. (17) also examined bleeding rates but did not mention whether these were managed conservatively or required intervention. Re-bleeding rates for trainees ranged from 0–3.8% compared to 0–3.4% for consultants in these 3 studies.
Operating time
Seven studies assessed the impact on trainee involvement on operating time (12,13,15,16,18-20). Five of these studies (12,15,16,18,20) found that there was a significant increase in operating time among trainees compared to consultants.
Operating times for trainees ranged from 85–136 min compared to 72–126 min for consultants. Reinisch et al. (19) and Uecker et al. (13) reported no significant differences in operating times between trainees and consultants.
Discussion
This systematic review examined the impact of trainee involvement on clinical outcomes in thyroid surgery. Due to the heterogeneity of the studies included, a meta-analysis was not performed. Despite this, this review has provided a narrative review illustrating that trainee involvement under supervision does not have a significant effect of hypocalcaemia rates, nerve injury and re-bleeding. In studies where operative time was assessed, this was found to be increased among trainees compared to consultants.
In the United Kingdom, the introduction of the European Working Time Directive (EWTD) has led to a perceived reduction in the operative experience that surgical trainees require in order to become competent in surgical procedures (21). It has also been reported that the changing work patterns has resulted in fewer operations being performed by junior and senior surgical trainees with a possible impact on clinical outcomes (22). The lack of operative exposure combined with working restrictions places emphasis on high quality training in order for surgical trainees to gain competencies. It has been suggested that high volume thyroid surgeons have better clinical outcomes compared to low volume surgeons (6,7) and having trainees rotate through these high-volume centres may improve their competencies without jeopardising patient outcomes. This was evident in the largest multicentre study included in this review where over 8,500 patients underwent total thyroidectomy (16). Twenty percent of these patients were operated on by trainees supervised by consultants, with no significant differences observed in clinically relevant outcomes.
The lack of training time implies that surgical training must be of the highest quality to ensure that trainees are exposed to a safe level of operating while maintaining low complication rates. Trainees performing complex operations such as thyroidectomies should be supervised by consultants to ensure that key steps of the operation are performed competently. Supervised operating also teaches the inexperienced trainee methods of identifying important structures such as the parathyroid glands and recurrently laryngeal nerve thus avoiding potentially life altering complications. In the current review, consultants/attendings were assisting/supervising their trainees and this may account for the low complication rates experienced by the trainee group and re-emphasises the need for trainee supervision to ensure a high quality of care is maintained.
Operating time was significantly longer in the trainee group compared to consultants. This finding is not only limited to trainee involvement in thyroid surgery as other reviews examining trainee involvement in other surgical specialties have replicated the same results (1,5). In the current review the maximum trainee operating time was 20 min longer that the consultant operating time with no significant impact on patient outcomes and should be expected as part of the trainees’ learning curve.
There are a few limitations of this review. There was degree of heterogeneity with the included studies. Eight of these studies were retrospective with the remaining 2 being prospective. Some studies examined hemithyroidectomies, while others looked at total thyroidectomies for both benign and malignant disease. A few studies did not explicitly define their outcome measures and all of studies were conducted in university affiliated hospitals which may limit the generalisability of the findings. Lastly, the degree of trainee involvement and supervision was not clearly defined in any of the included studies. Supervision can imply scrubbed in during the operation, not present but available when/if needed or assisting with only critical steps of the operation. This lack of information from the studies makes assessing the level of trainee involvement and supervision difficult to interpret.
Despite these limitations, this systematic review evaluated over 23,000 patients undergoing thyroid surgery, of which 11,000 were operated on by trainees. The results found no significant differences on hypocalcaemia, nerve injury or re-bleeding rates among trainees but did report a longer operating time. Trainee involvement in thyroid surgery with consultant supervision in high volume, dedicated teaching centres has no significant impact of patient outcomes.
Acknowledgments
We would like to acknowledge all the dedicate staff at the Royal Victoria Infirmary for their commitment to the patients under their care.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aot.2020.02.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Phillips AW, Dent B, Navidi M, et al. Trainee involvement in Ivor Lewis esophagectomy does not negatively impact outcomes. Ann Surg 2018;267:94-8. [Crossref] [PubMed]
- Saliba AN, Taher AT, Tamim H, et al. Impact of Resident involvement in Surgery (IRIS-NSQIP): Looking at the Bigger Picture Based on the American College of Surgeons – NSQIP Database. J Am Coll Surg 2016;222:30-40. [Crossref] [PubMed]
- Papandria D, Rhee D, Ortega G, et al. Assessing trainee impact on operative time for common general surgical procedures in ACS-NSQIP. J Surg Educ. 2012;69:149-55. [Crossref] [PubMed]
- Kasotakis G, Lakha A, Sarkar B, et al. Trainee participation is associated with adverse outcomes in emergency general surgery: an analysis of the National Surgical Quality Improvement Program database. Ann Surg 2014;260:483-90. [Crossref] [PubMed]
- Davis SS, Husain FA, Lin E, et al. Resident participation in index laparoscopic general surgical cases: impact of learning environment on surgical outcomes. J Am Coll Surg 2013;216:96-104. [Crossref] [PubMed]
- Adam MA, Thomas S, Youngwirth L, et al. Is there a minimum number of thyroidectomies a surgeon should perform to optimise patient outcomes? Ann Surg 2017;265:402-7. [Crossref] [PubMed]
- Al-Qurayshi Z, Robins R, Hauch A. Association of Surgeon Volume with outcomes and cost savings following thyroidectomy. A National Forecast. JAMA Otolaryngol Head Neck Surg 2016;142:32-9. [Crossref] [PubMed]
- American Association of Endocrine surgeons. Guiding standards for Successful completion of an AAES-Accredited Fellowship in Comprehensive Endocrine Surgery. Viewed 26 Oct 2019. Available online: www.endorcrinesurgery.org/curriculum
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the Prisma Statement. PLos Med 2009;6:e1000097. [Crossref] [PubMed]
- Slim K, Nini E, Forestier D, et al. Methodological index for non-randomised studies (minors):development and validation of a new instrument. ANZ J Surg 2003;73:712-6. [Crossref] [PubMed]
- Acun Z, Cihan A, Ulukent S, et al. A randomised prospective study of complications between general surgery residents and attending surgeons in Near-Total Thyroidectomies. Surg Today 2004;34:997-1001. [Crossref] [PubMed]
- Vieira BL, Hernandez DJ, Qin C, et al. The impact of resident involvement on otolaryngology surgical outcomes. Laryngoscope 2016;126:602-7. [Crossref] [PubMed]
- Uecker J, Luftman K, Ali S, et al. Comparable operative times with and without surgery resident participation. J Surg Educ 2013;70:696-9. [Crossref] [PubMed]
- Hassan I, Koller M, Kluge C, et al. Supervised trainees perform thyroid surgery for Graves Disease safely. Langenbecks Arch Surg 2006;391:597-602. [Crossref] [PubMed]
- Ambe PC, Wassenberg DR. Is sutureless thyroid surgery safe in the hands of surgical trainees. A single centre retrospective study. BMC Res Notes 2016;9:118. [Crossref] [PubMed]
- Gurrado A, Bellantone R, Cavallaro G, et al. Can Total Thyroidectomy Be safely performed by residents. Medicine (Baltimore) 2016;95:e3241. [Crossref] [PubMed]
- Mishra A, Agarwal G, Agarwal A, et al. Safety and Efficacy of Total Thyroidectomy in Hands of Endocrine Surgery Trainees. Am J Surg 1999;178:377-80. [Crossref] [PubMed]
- Emre AU, Cakmak GK, Tascilar O, et al. Complications of Total Thyroidectomy Performed by Surgical residents versus specialist surgeons. Surg Today 2008;38:879-85. [Crossref] [PubMed]
- Reinisch A, Malkomes P, Liese J, et al. Education in thyroid surgery: a matched-pair analysis comparing residents and board certified surgeons. Langenbecks Arch Surg 2016;401:239-47. [Crossref] [PubMed]
- Folsom C, Serbousek K, Lydiatt W, et al. Impact of resident training on operative time and safety in hemithyroidectomy. Head Neck 2017;39:1212-7. [Crossref] [PubMed]
- Giles JA. Surgical training and the European Working Time Directive:the role of informal workplace learning. Int J Surg 2010;8:179-80. [Crossref] [PubMed]
- Blencowe NS, Pasrson BA, Hollywoood AD. Effects of changing work patterns on general surgical trainng over the last decade. Postgrad Med J 2011;87:795-9. [Crossref] [PubMed]
Cite this article as: Ramsingh J, Truran P, Bliss R. A systematic review of trainee involvement in thyroid surgery and the impact on patient outcomes. Ann Thyroid 2020;5:2.


