Pre-operative optimization with super saturated potassium iodide solution (SSKI) in patients with graves’ disease undergoing total thyroidectomy
Introduction
For almost 100 years, iodine containing solutions have been utilized to help control hyperthyroidism for patients with Graves’ disease (1). The most current variation, super saturated potassium iodide solution (SSKI), is traditionally given about 10 days prior to surgery for patients with Graves’ disease to help control symptoms in addition to any other medication they may be taking for their symptoms (2). This was first noted by Plummer in 1913 with an effect coined by Drs. Jan Wolff and Israel Lyon Chaikoff, now known as the Wolff-Chaikoff effect (1). Surgeons have also noticed that pre-operative iodine solutions have helped assist with the technical aspects of the surgery, decreasing blood loss and improving the texture on the gland. Despite its widespread use, there is a limited amount of data supporting how SSKI affects the patient in the perioperative period (1-7). The 2016 ATA hyperthyroid guidelines supports that much of the limited literature is equivocal (8). The purpose of this study is to look at a single institution retrospective cohort comparing those patients who undergo thyroidectomy for Graves’ disease with the pre-operative administration of SSKI as compared to those who do not.
Methods
This is a single institution review of medical records with following parameters. Inclusion criteria are anyone who has Graves’ disease and has undergone a total thyroidectomy (ICD9 code = 242.0x OR ICD10 code = E05.0x with CPT code = 60240). Exclusion criteria were patients who had previous thyroid surgery. The study was IRB approved.
Data was collected regarding demographics including age, sex, body mass index (BMI), PMHx including COPD, CHF, MI, CKD, CVA. Previous treatment modalities were collected, including, previous use of propylthiouracil (PTU) and/or methimazole. Pre- and perioperative labs were collected including T3, and T4. The pre-operative lab was obtained 2–4 weeks before the operation prior to any administration of SSKI but after any adjustment of methimazole or PTU. The peri-operative values were all less than one week prior to the operation. Previous pre-operative ultrasound findings and which patients received SSKI were collected. In all patients, it was based on the surgeon’s preference about whether to order pre-operative SSKI. Intraoperative information such as the surgeon specialty who operated on the patient, intraoperative ultrasound findings, and gross intraoperative findings of the thyroid gland findings were collected. Post-operative complications as well including recurrent laryngeal nerve (RLN) injury, post-operative neck hematoma, and post-operative hypocalcemia were collected as well. Multivariate analysis was done analyzing the above demographics, PTU, methimazole, SSKI, gland size, and operative time.
Statistical analysis
The results of the study were analyzed using Excel 2013 (2013 Microsoft Corporation) and JMP. Comparisons were done using t-test and Chi-square to determine the relationship of means between groups. Multivariate analysis was done using ANOVA. For all data analyzed, the 95% confidence interval was computed with a resulting P value of ≤0.05 being considered statistically significant.
Results
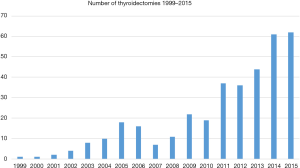
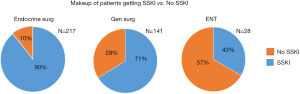
A total of 386 patients were identified with Graves’ disease who underwent an operation between 1999–2016. The number of cases increased dramatically per year from 1999 to 2016 likely due to the culture shift in realizing the benefit of performing total thyroidectomy in contrast to radioactive iodine ablation (RAI) or medical treatment (Figure 1). A total of 308 (79.8%) received SSKI prior to operation. Between the SSKI vs. non-SSKI groups, there was no significant difference between the demographics (see Table 1). Both groups had no statistical difference between use of PTU (25% vs. 15%, P=0.1) or methimazole (94% vs. 92%, P=0.9). The majority were operated on by endocrine surgeons 217 (56.2%), with the remaining being general surgeons 141 (36.5%) and ENT 28 (7.3%) (Figure 2).
Table 1
| Updated | SSKI [%] | Non-SSKI [%] | P value |
|---|---|---|---|
| Number | 308 | 78 | |
| BMI | 28.4 | 28.1 | 0.6 |
| Age, years | 43.2 | 46.3 | 0.07 |
| Sex (F) | 263 [85] | 65 [83] | 0.8 |
| COPD | 38 [12] | 12 [15] | 0.5 |
| CHF | 16 [5] | 6 [8] | 0.4 |
| MI | 3 [1] | 0 [0] | 0.2 |
| CKD | 8 [3] | 3 [4] | 0.5 |
| CVA | 8 [3] | 0 [0] | 0.2 |
| Smoking | 172 [56] | 35 [45] | 0.1 |
| PTU | 76 [25] | 12 [15] | 0.1 |
| Methimazole | 290 [94] | 72 [92] | 0.9 |
| Operative time (minutes) | 201 | 175 | <0.01 |
| Estimated blood loss (mL) | 39.1 | 37.6 | 0.9 |
| % cases with 100 mL or > EBL | 11.7% | 13.6% | 0.7 |
| Gland size (g) | 43.2 | 38.8 | 0.4 |
BMI, body mass index; PTU, propylthiouracil; COPD, chronic obstructive pulmonary disease; CHF, congestive heart failure; MI, myocardial infarction; CKD, chronic kidney disease ; CVA cerebrovascular accident; EBL, estimated blood loss; SSKI, super saturated potassium iodide solution.
Patients who received SSKI had no statistical different complication rates for persistent hypocalcemia 2.5% vs. 1.2% (P=0.3) or neck hematoma 1.3% vs. 2.5% (P=0.7). The rate of RLN injury was 0% for patients who received SSKI vs. 2.5% (P=0.04) for those who did not.
There was no statistical difference in the estimated blood loss of 39.1 mL as compared to 37.6 mL (P=0.9). The percent of cases with significant blood loss, determined as ≥100 mL was also not statistically different at 11.7% vs. 13.6% (P=0.7). Gland size was not statistically different between the groups, being 43.2 gm for the SSKI group compared to 38.8 gm in the non-SSKI group (P=0.4).
Patients who received SSKI had a significant drop in their baseline free T3 and free T4 levels to their immediate pre-op levels (while on SSKI) from pre-T3 value of 9.14 to 3.9 (P<0.001) and T4 of 2.76 to 1.39 (P<0.001) (see Figure 3).

On multivariate analysis, most factors were not statistically significant on estimated blood loss. The only factors that influenced blood loss were direct relationship with gland size and blood loss and the absence of SSKI increasing blood loss(P<0.05).
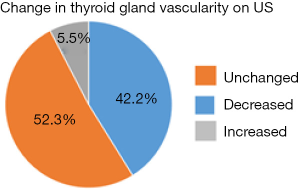
A total of 143 patients who received SSKI had peri-op and intra-op ultrasound with interpretable data. Fifteen patients had no increased flow on their initial ultrasound. Of the remaining 128, 54 (42.2%) had decreased flow, 67 (52.3%) had no change in flow, and 7 (5.5%) had increase in flow (see Figure 4). When rated on a scale of 0 (no flow) to 3 (markedly increased flow), there was an average flow of 2.0 on the preoperative flow which decreased to 1.5 on the intraoperative ultrasound, for a statistically significant decrease in flow of 25% (P<0.01).
Discussion
Graves’ disease is the most common form of hyperthyroidism, making up over half of all cases (9). Production of antibodies stimulating the thyrotropin receptor on thyroid cells causes the hyperthyroid state (9). Graves’ also produces exophthalmos and dermatopathy (9).
There are three mainstay treatments of Graves’ disease available to patients. The first is thyroid suppressing medication such as methimazole and PTU. These medications are effective in rendering the patient euthyroid, although only about 30–40% remain euthyroid off medication after a decade (9). These medications can have several severe side effects such as agranulocytosis, while rare, limit their protracted use (9).
The second is treatment with RAI. This is the most common form in the US and is treated with an ablative dose of I131 (9). While effective, there are limitations of this treatment. Exophthalmos may worsen with treatment of RAI (9). Compressive symptoms from enlarged goiter often do not improve (9). Recent evidence also suggests that patients with thyroid nodules will have unreliable biopsies after RAI, necessitating ultimately hemi- or total-thyroidectomy. RAI can cause xerostomia. RAI cannot be performed in pregnancy, large gland, those with ophthalmia, or those with nodules. Also there are patients who fail this treatment.
Third, total thyroidectomy can be performed. This is often the most definitive treatment for Graves’ disease (9). It will not worsen exophthalmos, can be safely performed during pregnancy, and can concomitantly treat compressive goiter and thyroid nodules. While the risk of temporary hypoparathyroidism can be high, 25% or greater, the rate of long term hypoparathyroidism is low in experienced hands (10). The risks of post-op injury to the RLN exist but are also low in the hands of experienced surgeons.
Two of the most pressing historical concerns about treatments patients with Graves’ disease are the risks of bleeding and the risks of peri-operative thyroid storm (9). The thyroid is a very vascular organ that over a century ago had unacceptably high morbidity and mortality due to blood loss. With improved surgical technique this has become an obsolete concern, however Graves’ disease thyroids are particularly hypervascular when compared to euthyroid patients (3,5). Peri-operative hyperthyroidism is of serious concern considering the hyperdynamic potential of patients with significantly elevated levels, especially intraoperatively.
The former Lugol’s agent, which was iodine suspended in alcohol, or the current supersaturated potassium iodine (SSKI) has been utilized to help render patients euthyroid perioperatively (11). This has been attributed to the Wolff-Chaikoff effect of saturating and down regulating the iodine receptors. It is usually given 10–14 days preoperatively. This can be seen to have a faster effect even with the concomitant use of methimazole (12). This also has been noted to decrease vascularity in the gland which assists with surgery. Despite its historic use, there has been limited and conflicting hard data supporting its clinical benefit. A few studies have demonstrated decreased vascularity and small operative benefits (4,10). There have been other studies with mixed results (6,7), or those suggesting that it may not have any increased benefit for pre-operative optimization (13,14). The current 2016 ATA guidelines mention it as a possible way to prepare patients for total thyroidectomy, but states that the literature is equivocal on its effects (8).
This paper follows previous papers that SSKI can improve pre-operative hormonal status and decreases vascularity in the thyroid gland. It appears that RLN injury may also be reduced, however it should be noted that this is still a very rare event with an overall occurrence of 0.5%. The very low rate in the paper may be due a slight underdiagnosis as it is only reported if it is either noted at the time of surgery or if a patient is having persistent symptoms. Asymptomatic or minimally symptomatic patients may not have been diagnosed properly since they may not have been aggressively diagnosed. It also shows on multivariate analysis to decrease estimated blood loss when other factors are controlled. These factors appear to be most apparent when the patient has significant vascularity or elevated hormone levels.
There were several limitations to this paper. First, a retrospective review, not all the data was available for all patients with Graves’ disease, especially hormonal labs and ultrasound results. Second, even though a statistically significant percentage of patients had a decrease in their vascularity, a majority had no documented change. This may be due to the qualitative and not quantitative measurements of blood flow change. It has been documented in a small randomized control trial that the quantitative blood flow through the thyroid gland does decrease with the administration of SSKI by almost 50% (3). Third, the decision to give SSKI was purely based on the discretion of the operating surgeon. While the standard care for the endocrine surgery department is to give SSKI to all patients, other surgeons may have had different criteria for pre-operative SSKI administration.
In conclusion, we believe that our study follows previous finds pre-operative SSKI likely improves patients peri-operatively with planned total thyroidectomy for Graves’ disease. It both decreases their hormonal levels of T3 and T4 and decreases the vascularity in the gland.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aot.2019.03.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Individual informed consent was waived due to the retrospective nature of the study. This study was approved by the Cleveland Clinic IRB (No. 16-1344).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Marigold JH, Morgan AK, Earle DJ, et al. Lugol's iodine: its effect on thyroid blood flow in patients with thyrotoxicosis. Br J Surg 1985;72:45-7. [Crossref] [PubMed]
- Kaur S, Parr JH, Ramsay ID, et al. Effect of preoperative iodine in patients with Graves’ disease controlled with antithyroid drugs and thyroxine. Ann R Coll Surg Engl 1988;70:123-7. [PubMed]
- Erbil Y, Parr JH, Ramsay ID, et al. Effect of Lugol Solution on Thyroid Gland Blood Flow and Microvessel Density in the Patients with Graves’’ Disease. J Clin Endocrinol Metab 2007;92:2182-9. [Crossref] [PubMed]
- Whalen G, Sullivan M, Maranda L, et al. Am J Surg. Randomized trial of a short course of preoperative potassium iodide in patients undergoing thyroidectomy for Graves' disease. Am J Surg 2017;213:805-9. [Crossref] [PubMed]
- Ansaldo GL, Pretolesi F, Varaldo E, et al. Doppler evaluation of intrathyroid arterial resistances during preoperative treatment with Lugol’s iodide solution in patients with diffuse toxic goiter. J Am Coll Surg 2000;191:607-12. [Crossref] [PubMed]
- Yabuta T, Ito Y, Hirokawa M, et al. Preoperative administration of excess iodide increases thyroid volume of patients with Graves’ disease. Endocr J 2009;56:371-5. [Crossref] [PubMed]
- Coyle PJ, Mitchell JE. Thyroidectomy: is Lugol’s iodine necessary? Ann R Coll Surg Engl 1982;64:334-5. [PubMed]
- Ross DS, Burch HB, Cooper DS, et al. 2016 American Thyroid Association Guidelines for Diagnosis and Management of Hyperthyroidism and Other Causes of Thyrotoxicosis. Thyroid 2016;26:1343-421. [Crossref] [PubMed]
- Weetman AP. Graves’ disease. N Engl J Med 2000;343:1236-48. [Crossref] [PubMed]
- Randle RW, Bates MF, Long KL, et al. Impact of potassium iodide on thyroidectomy for Graves' disease: Implications for safety and operative difficulty. Surgery 2018;163:68-72. [Crossref] [PubMed]
- Fischli S, Lucchini B, Müller W, et al. Rapid preoperative blockage of thyroid hormone production / secretion in patients with Graves’’ disease. Swiss Med Wkly 2016;146:w14243. [PubMed]
- Sato S, Noh JY, Sato S, et al. Comparison of efficacy and adverse effects between methimazole 15 mg+inorganic iodine 38 mg/day and methimazole 30 mg/day as initial therapy for Graves' disease patients with moderate to severe hyperthyroidism. Thyroid 2015;25:43-50. [Crossref] [PubMed]
- Shinall MC Jr, Broome JT, Baker A, et al. Is potassium iodide solution necessary before total thyroidectomy for Graves disease? Ann Surg Oncol 2013;20:2964-7. [Crossref] [PubMed]
- Shinall MC Jr, Broome JT, Nookala R, et al. Total thyroidectomy for Graves' disease: compliance with American Thyroid Association guidelines may not always be necessary. Surgery 2013;154:1009-15. [Crossref] [PubMed]
Cite this article as: Reznick D, Berber E, Jin J, Shin J, Siperstein A. Pre-operative optimization with super saturated potassium iodide solution (SSKI) in patients with graves’ disease undergoing total thyroidectomy. Ann Thyroid 2019;4:7.