Training and learning curve of intraoperative neuromonitoring
The early identification of laryngeal nerves has been accepted as the safest technique to reduce recurrent morbidity, but the identification of the nerve alone cannot ensure the presence of the function, because it is evident that the visual and anatomical integrity of the nerve does not always correspond to a normal function.
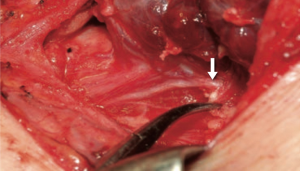
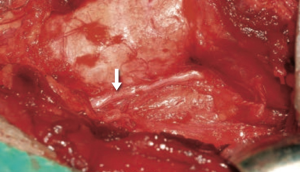
To confirm this, some studies have revealed that the most frequent cause of recurrent laryngeal nerve (RLN) injury during thyroid or parathyroid surgery is traction (70–96%), whose result is a suffering, often temporary transitory, of the RLN associated with complete anatomical integrity (1,2) (Figures 1,2).
Moreover, identification may not be easy, as in cases of reoperation, removal of central lymph nodes, thyrotoxicosis and in case of retrosternal goiter, thyroiditis or aberrant anatomy. Therefore it may be very useful to have an instrument that facilitates the safe completion of this important surgical step. For this reason, in recent years intraoperative neuromonitoring (IONM) has been proposed and applied in many centers in thyroid surgery in addition to the standard practice of visual identification of RLN, with the primary purpose of evaluating its function and facilitating its 'identification and dissection.
This work shows the benefits of the IONM technique (Figure 3), while recognizing that this technique cannot replace the fundamental elements in the performance of thyroidectomy: the usual visual identification of the RLN, the knowledge of the anatomical variables, the experience and the indispensability of pre- and postoperative laryngoscopy. However, before describing these benefits, it is useful to focus on the bibliographic data already existing in the literature regarding the scientific validation of this technique and on its ability to reduce RLN lesions during thyroidectomy.
It is now universally recognized that the best methodology to demonstrate the validity of one technique over another is the use of randomized prospective studies. However, with regard to the IONM technique, there are “natural” limitations to the implementation of this study methodology. The execution of randomized studies on this topic is in fact characterized by an important limitation in the statistical power, due to the substantial rarity of the complication (recurrent paralysis). In fact, it has been proven that, in order to validate the use of the IONM system, a multicentric experimentation is required with numerous and well-defined groups (3). In this respect, Dralle et al. said that to demonstrate a reduction in RLN paralysis from 2% to 1%, a study group of about 1,000 patients would be needed (4). Moreover, the conduct of these randomized prospective trials with at least two groups—IONM system compared with visual identification only—does not meet with the consensus of participation by the patients and by the surgeons themselves, due to the reluctance to participate in the group with the only visual identification. Despite these limitations in the literature, positive data on the IONM technique seem to emerge. In fact, through a prospective randomized study on 1,000 nerves at risk, Barczynski et al. have demonstrated that, using IONM, the prevalence of transient paresis of RLN was respectively 2.9% lower in high-risk patients (during tumor surgery with removal of paratracheal lymph nodes or in case of thyroidectomy for thyrotoxicosis or retrosternal goiter or in case of thyroiditis) and 0.9% in low-risk patients (non-toxic goiter surgery without retrosternal extension) (5).
Thomusch et al., reporting the results on a large series (over 5,000 thyroidectomies), concluded that the IONM of the RLN in thyroid surgery should be recommended because it is associated with a significantly lower incidence of transient or permanent palsies of the RLN (of 1.4% and of 0.4% respectively), compared to conventional visual identification (2.1% and 0.8%) (6). Furthermore, multivariate logistic regression analysis confirmed that the use of the IONM system significantly decreased the risk of temporary or permanent postoperative palsies of the RLN with a relative risk of 0.58 and 0.30 respectively.
Benefits of the IONM technique
Aid in identifying the RLN
The early and definitive identification of the RLN can minimize the risk of one of its lesions. The IONM technique can facilitate the localization of the RLN before its display and this is supported by the publication of multiple studies that confirm its effectiveness, with percentages very close to 100% (7). The RLN is detected in the paratracheal region by probe stimulation and subsequently visually identified by direct dissection based on the previous neural mapping. The IONM system helps to distinguish vessels from the nerves; therefore, once the nerve has been identified, further stimulation of the adjacent non-neural tissue compared to the nerve can aid in tracing both the nerve (positive signal) and the structures not as nervous as the vessels (no signal) (8).
Assistance in surgical dissection
During a thyroidectomy, a fundamental requirement is to obtain the greatest possible clarity of the anatomy of the RLN (position and anatomical variants), for the protection of the nerve (9). Once the nerve has been identified, further stimulation of adjacent non-neural tissue to the nerve may help to trace the nerve and all related branches through the dissected field, helping to distinguish between motor and sensitive branches. Electrical stimulation during thyroid surgery provides a functional view to the anatomy of the recurrent nerve. Some authors have suggested—using neural monitoring—two different conditions, from the prognostic point of view, of RLN suffering: segmental and global lesions. Through the use of the IONM, it has also been shown that the terminal ramifications of the RLN often have different functions: in particular, the anterior fibers are the driving fibers (positive signal) and the posterior ones are sensory. Via electrical stimulation, the ramifications of the constrictors of pharynx, larynx, trachea and cervical esophagus can also be identified (10).
Utility in the intraoperative diagnosis of RLN lesions, prognostic evaluation of postoperative neural function and identification of lesion site
Given the frequent bilateral nature of the classical thyroid procedure this aspect is remarkably significant for the prevention of bilateral paralysis of the vocal cords. The electrical examination of the nerve represents a significant improvement in the accuracy of the prognostic evaluation of the neural function compared to the simple visual inspection (11). The causes of injury to the RLN are various and most of them derive from accidents related to the surgical technique, such as the section of the nerve, the entrapment of the RLN by accidental ligation, the traction during the medicalization of the thyroid lobe, the lesions caused by the clamps, aspiration too close to the nerve, compression, contusion, pressure, ischemia due to excessive dissection and electrical/thermal injuries from instruments for hemostasis and dissection applied too close to the laryngeal nerve (12). Numerous studies have shown that even very experienced surgeons underestimate the actual lesions of the RLN. The percentage of intraoperative evidence of RLN lesions (when the surgeon is aware of the nerve injury during surgery) was estimated to be between 7.5% and 15%. Thus approximately 85–90% of recurring lesions are not perceived during surgery (13,14) (Table 1). The invisible lesions of the RLN (for example the thermal ones, from traction, compression, contusion or pressure) are not perceived by the surgeon's eyes (15); only a functional evaluation of the RLN via the IONM system can highlight such offended parts (Figures 1,2). The new devices for hemostasis and dissection, which release thermal or other energy and are widely used in modern operating rooms, can produce invisible collateral/proximal iatrogenic thermal lesions of adjacent structures, such as in laryngeal nerves (16). The IONM system assists in the intraoperative demonstration of functional loss of the RLN even when the nerve is visually intact. This intraoperative evaluation of the functionality of RLN by IONM during thyroid surgery is important for several reasons (17,18):
Table 1
| Authors | Injury [%] |
|---|---|
| Bergenfelz et al., Langenbencks Arch Surg 2008 | 1/10 [10] |
| Chiang et al., Surgery 2005 | 3/40 [7.5] |
| Lo et al., Arch Surg 2000 | 5/33 [15] |
| Patlow et al., Ann Surg 1986 | 1/10 [10] |
| Caldarelli et al., Otolaryngol Clin North Am 1980 | 1/10 [10] |
RLN, recurrent laryngeal nerve; IONM, intraoperative neuromonitoring.
- It allows intraoperative prediction of postoperative RLN functions (prognosis);
- It can prevent bilateral lesion of RLN by two-stage thyroidectomy (stage thyroidectomy);
- The IONM system accurately identifies the position of the interruption in nerve conduction by identifying how and when the RLN was injured;
- It facilitates the early differentiation between the alterations of the timbre of the voice whether connected or not to the RLN;
- Helping to identify the mechanism of RLN injury, it facilitates the surgeon to refine the surgical technique, reducing the mechanical trauma and the rate of paralysis of the nerves.
Improve the completeness of total thyroidectomy
Much of the difficulty in performing a total thyroidectomy occurs when the thyroid tissue is separated into the Berry ligament region. This difficulty is a frequent cause of accidental injury to the RLN, which is more damaged in the last 2 cm of its cervical course. The branching of the RLN often occurs less than 0.5 cm from the entrance of the larynx near the Berry ligament. The bifurcated RLN is also particularly prone to injury near the Berry ligament. At this level, the RLN can also have an intracapsular course in 10% of cases, according to Berlin (19), in 15% of the cases according to Armstrong et al. (20) and in 38% according to Wafae et al. (21). Therefore, to allow complete and safe re-section in a total thyroidectomy procedure during dissection at the Berry’s ligament, the surgeon needs a lot of attention, excellent exposure and neurophysiological confirmation of an intact nerve with the IONM system. Also the eventual haemostasis maneuvers of this area are better controlled by IONM; the indiscriminate use of clamps and electrocautery would most likely cause a nerve injury. Furthermore, maneuvers to minimize the risk of injury include an active awareness of the degree and duration of traction (22).
Use in endoscopic thyroidectomy
Laryngeal palpation (tactile sensation) or the use of magnifying glasses for the identification of the RLN or of the external branch of the superior laryngeal nerve (BENLS) is not feasible during endoscopic thyroidectomy because of the reduced incision or remote cervical access (breast approach and transaxillary thyroidectomy) (23). Endoscopic thyroidectomy (endoscopic thyroidectomy, ET) requires the surgeon to rely completely on the visual cues of a monitor. The magnification of the image provided by the new high-definition endoscopes facilitates the identification of the laryngeal nerve and the parathyroid glands, allowing also a visual discrimination between different tissues and depths. The use of the IONM system in ET is not only feasible but it is also easy, safe and effective, and helps visual identification of the nerves in the different minimal accesses of thyroid procedures (24); a standardized IONM technique with vagal stimulation was also proposed in the ET. The use of the IONM system in the ET does not produce an increase in the length of the surgical incision nor the operative time. The narrow working space and the possible problems related to the size and structure of a specific endoscopic instrumentation used to operate the neck do not seem to have negative effects on the use of this technique. The flexible tip of the monopolar stimulation probe provides excellent access to neural structures in areas outside the surgeon’s field of vision. The IONM system is complementary to video-endoscopic enlargement and helps the surgeon to feel more comfortable and confident in the initial approach especially to ET procedures. The same stimulator is useful to indicate the correct dissection plane, since it constantly provides information on the functioning of the laryngeal nerve during the operation and probably reduces the conversion rate relative to the conventional open technique. Furthermore, the IONM system has improved the identification of BENLS in the ET significantly.
Benefits for the trainee and the less experienced surgeon
Discussions are underway on the appropriateness of the use of new equipment, such as IONM, by trainees during their training in surgery (25). In fact, monitoring cannot be considered a substitute for a detailed knowledge of the anatomy of the thyroid gland and the surrounding tissue (26). Nevertheless, the IONM system of the RLN is a useful educational support for the trainee who approaches new devices, the standardized technique of thyroidectomy with vagal stimulation, the identification of RLN, anatomy, neurophysiology and pathophysiology of RLN. Furthermore, knowledge by IONM of the nerve injury mechanism during thyroidectomy is very instructive for the trainee for future operations. Knowledge of the intraoperative mechanism of RLN injury helps the surgeon to better refine the surgical technique, thus reducing both mechanical trauma and the rate of paralysis of the nerves (27). The multitude of research articles on simulation in surgical selection and training and a recent Cochrane review highlight the interest and wide application of simulated methods that can be utilized. A systematic review identified over 30 randomized controlled trials looking at surgical simulation. Simulation in surgical practice includes both operative and non-operative models and may incorporate multi-speciality and multi- disciplinary scenarios (28).
Dralle et al. described the risk factors of paralysis of the vocal cords after IONM of the RLN compared to the visual recognition and non-identification of the RLN in about 30,000 RLN at risk of injury: among the less experienced surgeons (with lower volume of treatments) the IONM of the RLN significantly reduced the frequency of permanent paralysis of the RLN (29).
NIM™ SAM-T represents the first IONM simulator for thyroid surgery (Figure 4). NIM™ SAM-T is a teaching and demonstration tool used to illustrate basic and advanced principles of nerve monitoring to medical professionals (30). It can be specifically used to: (I) demonstrate proper NIM™ set-up, (II) demonstrate different latencies associated with VN, RLN, and SLN; (III) simulate surgical effects of amplitude and latency to VN with the APS™; (IV) illustrate proper placement of EMG tubes; (V) demonstrate technique and proper placement of APS™ electrode; (VI) differentiate responses of the NIM™ (metal on metal artifact, train response below threshold, train response above threshold, stimulation artifact, far-field responses); (VII) demonstrate new features associated with latest NIM SW™ release V2.1.
The SAM-T system demonstrates the typical responses of the NIM™ system to different nerve stimuli encountered in the OR. While the experience is life-like, it is a simulation based on an extensive library of waveforms programmed into the SAM-T system. This unique feature allows SAM-T to demonstrate common stimulus responses (ex. amplitude change due to stretch of nerve tissue while dissecting at Ligament of Berry) by manually adjusting latency and amplitude with the turn of the corresponding knobs on the SAM-T control box. Trainees are keen to emphasize that simulation is only an adjunct to and not a replacement for clinical operative training (31).
Medical-legal aspects
There are few data, specifically medico-legal, on the use of the IONM system in thyroid surgery. However, the introduction of the same IONM system as a complement to the thyroidectomy procedure may also have useful implications from a medico-legal point of view (32).
Reduction of bilateral paralysis of the RLN
It is considered an important benefit in the modern era of thyroid surgery. If a total thyroidectomy has been planned, the possibility of knowing intraoperatively whether a nerve is injured or not makes it possible to make decisions about whether to proceed to the opposite side, then to complete thyroidectomy (33). The IONM system allows the surgeon to avoid contralateral lobe surgery if the first RLN has been diagnosed, thus avoiding the potential bilateral paralysis of the vocal cords which causes most of the disputes in thyroid surgery (34).
Documentation
Modern surgery is also documentation. The IONM system transforms muscular activity into recordable electromyographic signals that can be printed, archived and entered into the medical record. The documentation of the normal neurophysiological signals of the RLN at the end of the surgical procedure may have a forensic function, allowing the differentiation of the change in the tone of the voice linked to the RLN or not. The EMG signal is used as a test of intact nerve function at the end of the procedure. Some authors have stated that nerve monitoring during surgical procedures could reduce the medico-legal responsibility of surgeons, and also reduce economic losses to the health care system and insurance (35).
Difficult cases
It has been extensively demonstrated in prospective randomized studies that the IONM system produces significant benefits in difficult cases, such as iterative surgery, Graves’ disease, advanced thyroid cancer and undersea goiter. Today, therefore, it is difficult to justify the non-use of the IONM in difficult cases (36).
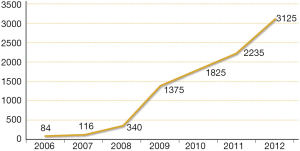
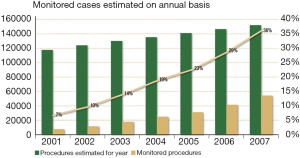
Standard of care in thyroid surgery
The causes of malpractice (especially in the United States) derive from the violation of standards of care; if, for example, a surgeon offers services below the standards to a patient who is damaged, in these cases it is very likely that the surgeon loses the cause. The standard of care is defined as the minimum cure that another doctor would provide in the same area (32,37). The following questions are of particular importance: what constitutes the standard management of RLN in the modern era of thyroid surgery? What is the current prevalence of IONM in thyroid surgery? How many surgeons use the IONM of the RLN? It has been reported that more than 45% of otolaryngologists use the IONM of the RLN and that 37% of the general surgeons who attended the American Association of Endocrine Surgery in 2006 used the IONM of the RLN (38) (Figures 5,6); the young surgeons and university surgeons with high percentage of cases (which probably face even the most difficult cases) used the IONM system more frequently. This percentage rose from 7% to 37% between 2001 and 2007. In Germany, more than 85% of thyroidectomies are performed using the IONM system, while in Northern Europe this percentage is about 77% (Table 2, Figure 7). For this reason the IONM system could become the standard of cure for thyroidectomy in the near future, even if some economic and cost-benefit aspects have yet to be assessed in a definitive way. Care standards are subject to changes and new technologies have been proposed and applied in thyroid surgery. In this modern era of surgery, specialists must practice safe surgery and document the surgical procedure: all this can be achieved thanks to the use of the IONM system.
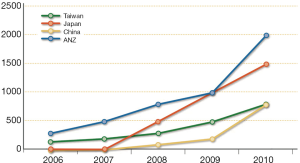
Table 2
| State | Thyroidectomy with IONM | Year | Reference |
|---|---|---|---|
| Denmark | 77% | 2007 | Goodballe C., ETA Meeting, Lisbona |
| Poland | 5% | 2010 | Barcinsky M., Polish Endocrine Surgeons |
| Germany | 87% | 2011 | Dralle H., Harvard Meeting, Boston |
| France | 6,200 | 2008 | Carnaille B, IONM study Group |
| 10,000 | 2010 | Carnaille B, IONM study Group | |
| Spain | 613 | 2009 | Manuel Poveda, Madrid 2011 |
| 1,956 | January–April 2011 | Manuel Poveda, Madrid 2011 |
IONM, intraoperative neuromonitoring.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Marcin Barczyński, Hui Sun and Xiaoli Liu) for the series “The Protection and Monitoring of Superior and Recurrent Laryngeal Nerve in Thyroid and Parathyroid Surgery” published in Annals of Thyroid. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aot.2019.02.01). The series “The Protection and Monitoring of Superior and Recurrent Laryngeal Nerve in Thyroid and Parathyroid Surgery” was commissioned by the editorial office without any funding or sponsorship. Gianlorenzo Dionigi serves as an unpaid editorial board member of Annals of Thyroid from Mar 2017 to June 2021. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the manuscript and ensure that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bergenfelz A, Jansson S, Kristoffersson A. Complications to thyroid surgery: results as reported in a database from a multicenter audit comprising 3,660 patients. Langenbecks Arch Surg 2008;393:667-73. [Crossref] [PubMed]
- Snyder SK, Lairmore TC, Hendricks JC, et al. Elucidating mechanisms of recurrent laryngeal nerve injury during thyroidectomy and parathyroidectomy. J Am Coll Surg 2008;206:123-30. [Crossref] [PubMed]
- Sturgeon C, Sturgeon T, Angelos P. Neuro-monitoring in thyroid surgery: attitudes, usage patterns, and predictors of use among endocrine surgeons. World J Surg 2009;33:417-25. [Crossref] [PubMed]
- Dralle H, Sekulla C, Lorenz KGerman IONM Study Group, et al. Intraoperative monitoring of the recurrent laryngeal nerve in thyroid surgery. World J Surg 2008;32:1358-66. [Crossref] [PubMed]
- Barczyński M, Konturek A, Cichon S. Randomized clinical trial of visualization versus neuromonitoring of recurrent laryngeal nerves during thyroidectomy. Br J Surg 2009;96:240-6. [Crossref] [PubMed]
- Thomusch O, Sekulla C, Walls G, et al. Intraoperative neuromonitoring of surgery for benign goiter. Am J Surg 2002;183:673-8. [Crossref] [PubMed]
- Timmermann W, Hamelmann WH, Thomusch O, et al. Effectiveness and results of intraoperative neuromonitoring in thyroid surgery. Statement of the Interdisciplinary Study Group on Intraoperative Neuromonitoring of Thyroid Surgery. Chirurg 2004;75:916-22. [Crossref] [PubMed]
- Yalçin B. Anatomic configurations of the recurrent laryngeal nerve and inferior thyroid artery. Surgery 2006;139:181-7. [Crossref] [PubMed]
- Lekacos NL, Tzardis PJ, Sfikakis PG, et al. Course of the recurrent laryngeal nerve relative to the inferior thyroid artery and the suspensory ligament of Berry. Int Surg 1992;77:287-8. [PubMed]
- Serpell JW, Yeung MJ, Grodski S. The motor fibers of the recurrent laryngeal nerve are located in the anterior extralaryngeal branch. Ann Surg 2009;249:648-52. [Crossref] [PubMed]
- Dionigi G. Energy based devices and recurrent laryngeal nerve injury: the need for safer instruments. Langenbecks Arch Surg 2009;394:579-80. [Crossref] [PubMed]
- Lahey FH, Hoover WB. Injuries to the recurrent laryngeal nerve in thyroid operations: their management and avoidance. Ann Surg 1938;108:545-62. [Crossref] [PubMed]
- Lo CY, Kwok KF, Yuen PW. A prospective evaluation of recurrent laryngeal nerve paralysis during thyroidectomy. Arch Surg 2000;135:204-7. [Crossref] [PubMed]
- Chang L, Petros J, Hess DT, et al. Integrating simulation into a surgical residency program: is voluntary participation effective? Surg Endosc 2007;21:418-21. [Crossref] [PubMed]
- Jatzko GR, Lisborg PH, Müller MG, et al. Recurrent nerve palsy after thyroid operations- -principal nerve identification and a literature review. Surgery 1994;115:139-44. [PubMed]
- Dionigi G, Boni L, Rovera F, et al. Neuromonitoring and video-assisted thyroidectomy: a prospective, randomized case-control evaluation. Surg Endosc 2009;23:996-1003. [Crossref] [PubMed]
- Chiang FY, Lu IC, Kuo WR. The mechanism of recurrent laryngeal nerve injury during thyroid surgery. The application of intraoperative neuromonitoring. Surgery 2008;143:743-9. [Crossref] [PubMed]
- Chiang FY, Wang LF, Huang YF, et al. Recurrent laryngeal nerve palsy after thyroidectomy with routine identification of the recurrent laryngeal nerve. Surgery 2005;137:342-7. [Crossref] [PubMed]
- Berlin D. The recurrent laryngeal nerve in total ablation of the normal thyroid gland. Surg Gynecol Obstet 1935;60:19-26.
- Armstrong WG, Hinton JW. Multiple divisions of the recurrent laryngeal nerve. An anatomic study. AMA Arch Surg 1951;62:532-9. [Crossref] [PubMed]
- Wafae N, Vieira MC, Vorobieff A. The recurrent laryngeal nerve in relation to the inferior constrictor muscle of the pharynx. Laryngoscope 1991;101:1091-3. [Crossref] [PubMed]
- Karlan MS, Catz B, Dunkelman D, et al. A safe technique for thyroidectomy with complete nerve dissection and parathyroid preservation. Head Neck Surg 1984;6:1014-9. [Crossref] [PubMed]
- Kruse E, Olthoff A, Schiel R. Functional anatomy of the recurrent and superior laryngeal nerve. Langenbecks Arch Surg 2006;391:4-8. [Crossref] [PubMed]
- Terris DJ, Anderson SK, Watts TL, et al. Laryngeal nerve monitoring and minimally invasive thyroid surgery: complementary technologies. Arch Otolaryngol Head Neck Surg 2007;133:1254-7. [Crossref] [PubMed]
- Parsons BA, Blencowe NS, Hollowood AD, et al. Surgical training: the impact of changes in curriculum and experience. J Surg Educ 2011;68:44-51. [Crossref] [PubMed]
- Bliss RD, Gauger PG, Delbridge LW. Surgeon’s approach to the thyroid gland: surgical anatomy and the importance of technique. World J Surg 2000;24:891-7. [Crossref] [PubMed]
- Hermann M, Alk G, Roka R, et al. Laryngeal recurrent nerve injury in surgery for benign thyroid diseases: effect of nerve dissection and impact of individual surgeon in more than 27,000 nerves at risk. Ann Surg 2002;235:261-8. [Crossref] [PubMed]
- Schijven MP, Jakimowicz JJ, Broeders IA, et al. The Eindhoven laparoscopic cholecystectomy training course--improving operating room performance using virtual reality training: results from the first E.A.E.S. accredited virtual reality trainings curriculum. Surg Endosc 2005;19:1220-6. [Crossref] [PubMed]
- Dralle H. Impact of modern technologies on quality of thyroid surgery. Langenbecks Arch Surg 2006;391:1-3. [Crossref] [PubMed]
- Gurusamy KS, Aggarwal R, Palanivelu L, et al. Virtual reality training for surgical trainees in laparoscopic surgery. Cochrane Database Syst Rev 2009;CD006575. [PubMed]
- Sutherland LM, Middleton PF, Anthony A, et al. Surgical simulation: a systematic review. Ann Surg 2006;243:291-300. [Crossref] [PubMed]
- Angelos P. Recurrent laryngeal nerve monitoring: state of the art, ethical and legal issues. Surg Clin North Am 2009;89:1157-69. [Crossref] [PubMed]
- Sancho JJ, Pascual-Damieta M, Pereira JA, et al. Risk factors for transient vocal cord palsy after thyroidectomy. Br J Surg 2008;95:961-7. [Crossref] [PubMed]
- Randolph GW. editor. Surgical anatomy of the recurrent laryngeal nerve. In Surgery of the thyroid and parathyroid glands. Elsevier Science, Philadelphia, 2003.
- Shaw GY, Pierce E. Malpractice litigation involving iatrogenic surgical vocal fold paralysis: a closed- claims review with recommendations for prevention and management. Ann Otol Rhinol Laryngol 2009;118:6-12. [Crossref] [PubMed]
- Kern KA. Medicolegal analysis in the diagnosis and treatment of surgical endocrine disease. Surgery 1993;114:1167. [PubMed]
- Lydiatt DD. Medical malpractice and the thyroid gland. Head Neck 2003;25:429-31. [Crossref] [PubMed]
- Horne SK, Gal TJ, Brennan JA. Prevalence and patterns of intraoperative nerve monitoring for thyroidectomy. Otolaryngol Head Neck Surg 2007;136:952-6. [Crossref] [PubMed]
Cite this article as: Pino A, Caruso E, Pontin A, Dionigi G. Training and learning curve of intraoperative neuromonitoring. Ann Thyroid 2019;4:2.