
The evolution and progress of intraoperative monitoring of the external branch of the superior laryngeal nerve in thyroid surgery
Introduction
Hypoparathyroidism and recurrent laryngeal nerve (RLN) damage are the most frequent reported morbidity in thyroid surgery (1,2). However, injury of the external branch of the superior laryngeal nerve (EBSLN) has been considered to be the most neglected complication with an estimate of an average prevalence far exceeding 20% (3,4). EBSLN injury results in subtle changes in voice as a result of dysfunction of the cricothyroid muscle (CTM): changed basic voice frequency, deterioration of voice quality in the production of high frequency sounds and reduced voice projection. The symptoms of this dysfunction are usually more notable for professional voice users. EBSLN damage can be uneasy to be recognized intraoperatively, and it is almost impossible to be revealed during routine postoperative laryngeal exam. More sophisticated exams such as videostrobolaryngoscopy or electromyography (EMG) of the CTM can help to establish this diagnosis (5). EBSLN injury can happen during dissection of the vessels of the upper thyroid pole due to proximity between the nerve and these vessels. Some individuals are at increased risk of EBSLN injury including those with a big tumor within the upper part of the thyroid lobe, large volume of the thyroid gland exceeding 100 mL or patients with a short neck in whom the nerve can descent close to or below the superior thyroid pole (Cernea type IIA or IIB). In these patients, the superior thyroid pole can located higher than usual and the nerve can be adherent to the thyroid as a result of this relative dislocation (3,4).
Several maneuvers have been implemented into surgical armamentarium to diminish the risk of EBSLN injury during management of the upper thyroid vessels:
- Meticulous and peri-capsular ligation of each of the branches of the upper thyroid vessels without visualization of the nerve (6,7);
- Visual inspection of the EBSLN before ligation of the upper thyroid pole vessels (8,9);
- Intraoperative neuromapping or neural stimulation technique for confirmation of the EBSLN revealing (5,10,11).
No versus visual identification of the EBSLN
In the past most surgeons tended to avoid rather than identify the EBSLN to assure its preservation during thyroid surgery. This surgical technique is based on meticulous and peri-capsular ligation of each of the branches of the upper thyroid vessels without visualization of the nerve. In this technique the EBSLN is not routinely exposed and the most distal 2.0 cm of the superior thyroid vessels are carefully dissected, exposed, and ligated separately as individual branches to ensure no entrapment of the nerve in the ligatures. Loré et al. has shown in a detailed subjective voice evaluation that utilization of this technique among 66 patients who underwent thyroid surgery 14 (21.2%) patients had notable changes including 9 temporary and 5 permanent events. However, these voice changes had no deleterious effect on lifestyle in 13 individuals, and the effects were indeterminate in 1 patient lost to follow-up (6). In addition, Bellantone et al. demonstrated in a randomized study comprised of 289 patients who were qualified for thyroidectomy and were randomly assigned into one of the 2 groups and followed-up with a phoniatric evaluation with videostrobolaryngoscopy and spectrographic examination afterwards: group A (215 nerves at risk), the superior thyroid vessels were ligated following visualization of the EBSLN, and group B (244 nerves at risk), the superior thyroid vessels were ligated using peri-capsular dissection technique of individual branches to assure EBSLN preservation without attempts to visually recognize the nerve before ligation, that the latter surgical manoeuver turned out to be a safe technique to prevent EBSLN injury. In this study in group A, in 11.6% of nerves at risk the EBSLN was not identified. The EBSLN function remained unaltered in both groups of patients during the entire 6-months follow-up postoperatively. However, mean operating time was significantly shorter for group B patient compared to group A individuals (7).
Neural monitoring of the EBSLN
In the recent guideline statement the International Neural Monitoring Study Group put special emphasis on the need of routine visual inspection for the nerve in all operations (2,5). Visual identification rate of the EBSLN at expert hands of thyroid surgeons was reported to be exceeding 98% (12). The EBSLN was found in this study using visual identification technique to be at high risk of injury (Cernea type 2b) in 48.3% of patients, and at low risk of injury (Cernea type 1) in 7.3% of individuals. Specimens larger than 100 g were correlated with type 2b nerves which are well-known to be at highest risk of injury (12). However, in most published studies visual inspection of the EBSLN in not possible in more than two-thirds of patients (10,13,14). In addition, Friedman et al. found that almost 20% of EBSLNs were not eligible for visual identification owing to their subfasical or intramuscular course (9,15). In addition, Selvan has reported that non-neural anatomical structures of regional musculature can be mistakenly identified as the EBSLN. Hence, the International Neural Monitoring Study Group has agreed upon recently that attempts to visually identify the EBSLN should be facilitated by implementation of neural stimulation technique with evaluation of at least CTM twitch response or preferably the glottis endotracheal EMG monitoring to assure functional preservation of the nerve during thyroidectomy (11).
As shown by data from the current international survey on the identification and neural monitoring of the EBSLN during thyroidectomy IONM was used for recognition of the EBSLN in the majority of patients by 5/19 (26.3%) low-volume vs. 39/57 (68.4%) highest-volume surgeons (>200 thyroidectomies per year) based on the CTM twitch assessment (P=0.004), and 3/16 (15.8%) low-volume vs. 35/57 (61.4%) highest-volume surgeons based on the evaluation of endotracheal surface EMG (P<0.001). Eight of nineteen (42.1%) low-volume surgeons vs. 39/57 (68.4%) highest-volume surgeons were aware of the EBSLN Neural Monitoring Guideline Statement (P=0.041) (16).
Barczynski et al. demonstrated in a randomized study comprising 210 patients who were randomized into two arms (n=105, each): visual identification of the EBSLN and RLN vs. additional EBSLN and RLN monitoring that use of IONM corresponded to the improved identification rate of the EBSLN during surgery (34.5% without IONM and 83.8% with IONM), as well as reduced incidence of transient EBSLN damage in latter group (5.0% vs. 1.0%, respectively; P=0.02), findings which correlated to the diminished risk of early phonation changes after surgery in the monitored arm (10). Similar conclusions were drawn by Uludag et al. based on the outcomes of a randomized study of 133 patients qualified for thyroidectomy who were randomized into 2 groups: group 1 (105 nerves at risk), upper thyroid pole dissection was done without visual identification of the EBSLN; and group 2 (106 nerves at risk), IONM was utilized to map out the EBSLN during thyroidectomy (14). The EBSLN Voice Impairment Index-5 (VII-5) served in this study during 6-months postoperative follow-up to reveal altered postoperative voice performance. EBSLN damage was diagnosed in nine (8.6%) nerves at risk in group 1 and in 1 (0.9%) nerve at risk in group 2 patients (P=0.015 and P=0.010, respectively). IONM was considered to markedly assist in both visual identification and functional neural preservation among group 2 patients in this study. The VII-5 revealed significantly altered voice in group 1 vs. group 2 during the entire 6-months postoperative follow-up period. Authors concluded that IONM plays a major role in functional preservation of the EBSLN leading to decreased rate of EBSLN damage during the upper thyroid pole management (14).
In addition, Masuoka et al. published recently outcomes of a prospective randomized study including 252 patients and focused on the EBSLN injury during thyroid surgery. In one arm of this study patients underwent surgery with IONM (group N operated on with NIM-Response 3.0 system) to facilitate localization of the EBSLN and in the other arm IONM was not used and conventional surgical technique (group C operated on with conventional Vari-Stim 3 system) was utilized instead (17). Endpoints of this study were: the identification rate of the EBSLN (primary) and prevalence of postoperative voice alterations (secondary). Use of NIM Response 3.0 system improved 5-fold the identification rate of the EBSLN which was mapped out in the operative field more accurately using NIM system when compared to conventional Vari-Stim 3 system (89.2% vs. 17.8%, P<0.001) and reduced significantly cohort of female patients with postoperative subjective voice alterations (17).
Aina et al. also reported a very high proportion of patients equal to 92.7% who had the EBSLN identified intraoperatively during thyroid surgery owing to the use of a nerve stimulator. The identification of the nerve was successful in the majority of primary surgeries but it was positive only in two-thirds of the redo operations (8).
In Selvan’s study comprising of 70 nerves at risk the EBSLNs were successfully identified using nerve stimulation and the CTM EMG waveform analysis in all cases (11). However, the methodology of this study in which the nerve was initially identified visually and then confirmed by electrical testing allowed for revealing that visualization alone may be misleading in many cases. Surprisingly there were many false-positive identifications of the EBSLN in this study and electrical stimulation of the anatomical structures falsely estimated to be the EBSLN like non-neural fibers or tendinous fibers of the CTM or inferior constrictor muscles was the only way to make the definitive identification of the nerve with functional confirmation in CTM twitch and EMG response. Hence, visualization of the EBSLN alone without electrophysiological confirmation entails a serious risk of a false-positive identification and only implementing functional data to this surgical technique could make the nerve preservation more accurate and independent of the subjective surgical judgment (11).
Lee et al. reported recently interesting outcomes of a prospective study of 490 thyroid operations (299 total thyroidectomies and 191 hemithyroidectomies) with IONM used to facilitate RLN and EBSLN identification and preservation compared to outcomes of 500 thyroidectomies performed by the same surgeon without IONM (18). In this study demographic characteristics, type of operation, pathology, RLN and EBSLN identification and classification, together with some functional and electrophysiological data as well as surgical morbidity were analyzed. Interestingly, the added-value of IONM defined as improved identification rate of the EBSLN when compared to the visual inspection alone was in this study equal to 13.8% (P<0.0001) and this value was even higher and equal to 15.8% for type 2b EBSLN. Usefulness of IONM could not have been predicted by analysis of preoperatively known factors including indications for surgery. Hence authors concluded that routine utilization of IONM by high-volume thyroid surgeons allowed for better intraoperative management of the RLN and EBSLN over visual identification technique alone and attempts to pre-select patients for IONM selective use could not have been accurate based on operative indication (18).
Surgical technique of the EBSLN stimulation and monitoring
The International Neural Monitoring Study Group proposed recently an optimal management strategy of the superior thyroid pole dissection involving two maneuvers available only with neural stimulation or monitoring of the EBSLN to be maximally assured of the nerve preservation (5):
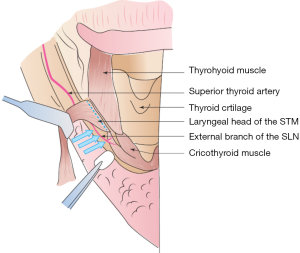
(I) The EBSLN should be stimulated with observation of the CTM twitch or endotracheal EMG waveform (if present) cranially and medial to the upper thyroid pole vessels (a true positive stimulation), as shown on Figure 1.
(II) Stimulation of the tissues neighboring the upper thyroid vessels before their division at the given level should be negative for EBSLN identification which means that there is no CTM twitch or endotracheal EMG waveform following this stimulation (a true negative stimulation).
Contrary to the RLN monitoring the EBSLN monitoring relies on evaluation of clearly visible CTM twitch (present in all patients following a positive identification of the nerve) and EMG glottis waveform analysis recorded by the surface endotracheal tube electrodes observable in the majority but not all patients (70–80%) when using standard EMG tubes or approaching to 100% of patients (using NIM TriVantage tubes, which have additional electrodes located on the anterior and more proximal surface of the tube to assure proximity to the CTM) (19,20). IONM of the EBSLN with EMG assessment provides the additional benefits for prognostication, quantification and documentation of neural function over solely stimulation of the nerve with CTM twitch assessment (21-24). It is advised that at the final stage of upper thyroid pole dissection the EBSLN should be stimulated at the most cranial arc of dissection to confirm not only anatomical but what is even more important functional preservation of intact neural function (5).
Conclusions
The surgeon should be familiar with all possible variations of EBSLN anatomy in the vicinity of the upper thyroid pole. Intraoperative stimulation of the EBSLN with or without nerve monitoring can improve the visual identification rate of the nerve, diminish both prevalence of nerve injury and postoperative voice impairment which have been repeatedly supported by recently published data.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Marcin Barczyński, Hui Sun, and Xiaoli Liu) for the series “The Protection and Monitoring of Superior and Recurrent Laryngeal Nerve in Thyroid and Parathyroid Surgery” published in Annals of Thyroid. The article has undergone external peer review.
Conflicts of interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aot.2018.10.01). The series “The Protection and Monitoring of Superior and Recurrent Laryngeal Nerve in Thyroid and Parathyroid Surgery” was commissioned by the editorial office without any funding or sponsorship. Marcin Barczyński served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Annals of Thyroid from Aug 2017 to Jul 2019. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the manuscript and ensure that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Barczyński M, Konturek A, Stopa M, et al. Total thyroidectomy for benign thyroid disease: is it really worthwhile? Ann Surg 2011;254:724-29. [Crossref] [PubMed]
- Randolph GW, Dralle HInternational Intraoperative Monitoring Study Group, et al. Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope 2011;121:S1-16. [Crossref] [PubMed]
- Cernea CR, Ferraz AR, Furlani J, et al. Identification of the external branch of the superior laryngeal nerve during thyroidectomy. Am J Surg 1992;164:634-39. [Crossref] [PubMed]
- Cernea C, Ferraz AR, Nishio S, et al. Surgical anatomy of the external branch of the superior laryngeal nerve. Head Neck 1992;14:380-3. [Crossref] [PubMed]
- Barczyński M, Randolph GW, Cernea CR, et al. External branch of the superior laryngeal nerve monitoring during thyroid and parathyroid surgery: International Neural Monitoring Study Group standards guideline statement. Laryngoscope. 2013;123:S1-14. [Crossref] [PubMed]
- Loré JM Jr, Kokocharov SI, Kaufman S, et al. Thirty-eight-year evaluation of a surgical technique to protect the external branch of the superior laryngeal nerve during thyroidectomy. Ann Otol Rhinol Laryngol 1998;107:1015-22. [Crossref] [PubMed]
- Bellantone R, Boscherini M, Lombardi CP, et al. Is the identification of the external branch of the superior laryngeal nerve mandatory in thyroid operation? Results of a prospective randomized study. Surgery 2001;130:1055-9. [Crossref] [PubMed]
- Aina EN, Hisham AN. External laryngeal nerve in thyroid surgery: recognition and surgical implications. ANZ J Surg 2001;71:212-4. [Crossref] [PubMed]
- Friedman M, Wilson MN, Ibrahim H. Superior laryngeal nerve identification and preservation in thyroidectomy. Operative Techn Otolaryngol 2009;20:145-51. [Crossref]
- Barczyński M, Konturek A, Stopa M, et al. Randomized controlled trial of visualization versus neuromonitoring of the external branch of the superior laryngeal nerve during thyroidectomy. World J Surg 2012;36:1340-7. [Crossref] [PubMed]
- Selvan B, Babu S, Paul MJ, et al. Mapping the compound muscle action potentials of cricothyroid muscle using electromyography in thyroid operations: a novel method to clinically type the external branch of the superior laryngeal nerve. Ann Surg 2009;250:293-300. [Crossref] [PubMed]
- Pagedar NA, Freeman JL. Identification of the external branch of the superior laryngeal nerve during thyroidectomy. Arch Otolaryngol Head Neck Surg 2009;135:360-2. [Crossref] [PubMed]
- Masuoka H, Miyauchi A, Higashiyama T, et al. Prospective randomized study on injury of the external branch of the superior laryngeal nerve during thyroidectomy comparing intraoperative nerve monitoring and a conventional technique. Head Neck 2015;37:1456-60. [Crossref] [PubMed]
- Uludag M, Aygun N, Kartal K, et al. Contribution of intraoperative neural monitoring to preservation of the external branch of the superior laryngeal nerve: a randomized prospective clinical trial. Langenbecks Arch Surg 2017;402:965-76. [Crossref] [PubMed]
- Lennquist S, Cahlin C, Smeds S. The superior laryngeal nerve in thyroid surgery. Surgery 1987;102:999-1008. [PubMed]
- Barczyński M, Randolph GW, Cernea C, et al. International survey on the identification and neural monitoring of the EBSLN during thyroidectomy. Laryngoscope 2016;126:285-91. [Crossref] [PubMed]
- Masuoka H, Miyauchi A, Yabuta T, et al. Innervation of the cricothyroid muscle by the recurrent laryngeal nerve. Head Neck 2016;38:E441-5. [Crossref] [PubMed]
- Lee J, Fraser S, Glover A, et al. Prospective evaluation of the utility of routine neuromonitoring for an established thyroid surgical practice. ANZ J Surg 2017;87:E138-42. [Crossref] [PubMed]
- Potenza AS, Phelan EA, Cernea CR, et al. Normative intra-operative electrophysiologic waveform analysis of superior laryngeal nerve external branch and recurrent laryngeal nerve in patients undergoing thyroid surgery. World J Surg 2013;37:2336-42. [Crossref] [PubMed]
- Darr EA, Tufano RP, Ozdemir S, et al. Superior laryngeal nerve quantitative intraoperative monitoring is possible in all thyroid surgeries. Laryngoscope 2014;124:1035-41. [Crossref] [PubMed]
- Hurtado-López LM, Díaz-Hernández PI, Basurto-Kuba E, et al. Efficacy of intraoperative neuro-monitoring to localize the external branch of the superior laryngeal nerve. Thyroid 2016;26:174-8. [Crossref] [PubMed]
- Glover AR, Norlén O, Gundara JS, et al. Use of the nerve integrity monitor during thyroid surgery aids identification of the external branch of the superior laryngeal nerve. Ann Surg Oncol 2015;22:1768-73. [Crossref] [PubMed]
- Potenza AS, Araujo Filho VJF, Cernea CR. Injury of the external branch of the superior laryngeal nerve in thyroid surgery. Gland Surg 2017;6:552-62. [Crossref] [PubMed]
- Sun H, Dionigi G. Monitoring the external branch of the superior laryngeal nerve in thyroid surgery. Ann Thyroid 2018;3:9. [Crossref]
Cite this article as: Barczyński M, Wojtczak B, Konturek A. The evolution and progress of intraoperative monitoring of the external branch of the superior laryngeal nerve in thyroid surgery. Ann Thyroid 2018;3:24.


