
Surgical anatomy for transoral endoscopic thyroid surgery through vestibular approach (TOETVA)
Introduction
Since American surgeon Michel Gagner accomplished the first endoscopic parathyroid surgery in 1996, endoscopy thyroidectomy (ET) has been widely applied for treatment of different thyroid diseases including nodular goiter, Graves’ disease and follicular tumors [benign tumors and suitable differentiated thyroid cancers (DTCs)] in the past 20 years. ET, especially scarless endoscopic thyroidectomy (SET), is popular mainly due to its perfect cosmetic effect. Various approaches have been introduced for performing SET, including extracervical access [anterior chest wall (1) and axilla (2)] and transoral access [sublingual (3) and vestibule (4,5)].
Extracervical access approach has been proved to be safe and can avoid the visible scar on the neck. However, it requires extensive flap dissection and is controversial on its enhanced physical trauma. Besides, inevitable scars are finally left on the body surface. Recently, natural orifice transluminal endoscopic surgery (NOTES) has generated excitement among surgeons as potentially scar-free surgery. Especially for thyroidectomy, transoral approach can be truly physical minimal invasive, safe and cosmetic effective. In 2008, the first clinical application of transoral thyroidectomy by the sublingual approach was reported by Witzel et al. (3), and the first vestibule approach by Nakajo (4). Currently, the vestibule access is preferred for transoral thyroidectomy (5).
Comparing to traditional extracervical approaches, Transoral endoscopic thyroid surgery through vestibular approach (TOETVA) requires “to see” the anatomical structures from an opposite direction. Therefore, the “up-down” vision of the traditional, well-known, surgical landmarks must be well understood by surgeons. Previous researches have studied anatomy under transoral perception on animals and cadavers (6-9). Here, we are going to summarize our experience of TOETVA on human from the vision of clinical anatomy.
The anatomy of oral vestibule
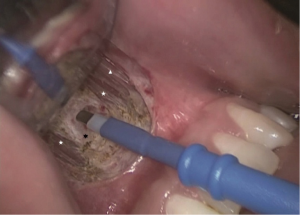
The oral vestibule is bounded anteriorly and laterally by the cheeks and the lips, and posteriorly and medially by the teeth and the gums. The lips are covered by skin externally and a mucous membrane internally. The most important landmarks of the oral vestibule in TOETVA are the mandibula labial frenulum and the mandibular first premolars (Figure 1). The labial frenulum is the median folds of the mucous membrane connecting the lips to the gum. The mandibular first premolar is the fourth mandible tooth from median line. In TOETVA, a 1cm horizontal incision is made across the mandibula labial frenulum, and is served as observation hole. Two 0.5-cm vertical incisions are made on the lip inferolateral to the mandibular first premolars, and are served as operating holes (Figure 2).


The mental nerve is a sensory nerve originating from the inferior alveolar nerve and contributes to the sensation of the oral vestibule. The mental nerve emerges at the mental foramen which is located below the root of the mandible second premolar. In TOETVA, the mental nerve is not routinely exposed. To avoid injury of the mental nerve, the 0.5-cm incisions, as is shown in Figure 1, should not be made closely to the root of the mandibular first premolars, and the 5-mm trocars should be moved directly downward, crossing the lower boundary of the mandible, before their direction turning internally.
As is shown in Figure 3, there are four major muscle upon the mandibule, including the orbicularis oris, the depressor labii inferioris, the mentalis and the depressor anguli oris (10). The orbicularis oris is an orbicular muscle that consists muscular fibers from different directions surrounding the orifice of the mouth and also fibers derived from the other facial muscles. The depressor labii inferioris arises from the oblique line of the mandible and passes upwards and medially into the skin and mucosa of the lower lip. It is located between the symphysis menti and the mental foramen and is continuous with the fibers of the platysma muscle at its origin. The mentalis is a paired central muscle originating from the incisive fossa of the mandible and inserting into the skin of the chin. The depressor anguli oris arises from the mental tubercle of the mandible and the oblique line below and lateral to depressor labii inferioris. Its fibers converge converges into a narrow fasciculus inserted into the angle of the mouth.

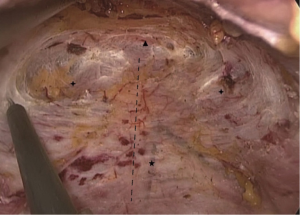
In TOETVA, dissection of the main tunnel is performed beneath these muscles and upon the periosteum of mandibule in order to decrease bleeding and prevent injury of these muscles (Figure 4). On the other side, these muscles are then connected to the platysma in the neck. Dissection closely to the periosteum can prevent skin injury and insure the working space to be beneath the platysma.
The anatomy of the submandibular space
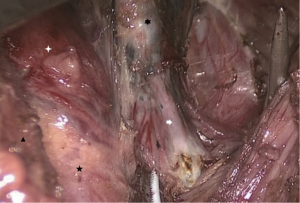
The submandibular space arises from the mandibule to the hyoid bone and is the channel for the three tunnels during TOETVA. The proper level for these three trocars is in the superficial level of deep cervical fascia, beneath the dorsal part of the platysma. It should be between the bilateral sternocleidomastoid muscles and upon the ventral part of suprahyoid muscles including the digastric muscle, the mylohyoid muscle, the geniohyoid muscle and the stylohyoid muscle (Figures 5,6) (10).
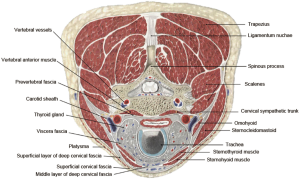
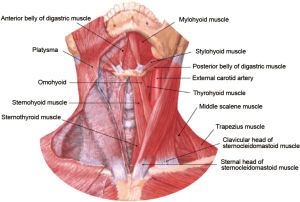
Important muscular structures at the submandibular space include the platysma, the sternocleidomastoid and the suprahyoid muscles. The platysma is a superficial muscle that arises from the fascia covering the upper parts of pectoralis major and deltoid. Its fibers mainly interlace with the fibers of the contralateral muscle across the midline. The rest fibers attach to the lower border of the mandible or to the lower lip or cross the mandible to attach to skin and subcutaneous tissue of the lower face. The sternocleidomastoid is a tricep that originates from the manubrium of the sternum and the clavicle. It travels obliquely upwards, and is inserted to the mastoid process of the temporal bone. The digastric muscle is composed of two bellies connected by an intermediate tendon which is attached to the body and greater cornu of the hyoid bone. It extends from the mastoid notch to the symphysis menti in a curved form. The mylohyoid muscle is located immediately superior to the anterior belly of the digastric muscle and runs from the mylohyoid line to the hyoid bone, forming the floor of the oral cavity. The geniohyoid muscle arises from the mental spine and is located superior to the medial border of the mylohyoid muscle. The stylohyoid muscle arises from the styloid process of the temporal bone, passing inferior and anterior and inserting into the body of the hyoid bone.
The key to prevent complications related to creating working space is to keep moving trocars in the right space mentioned above (Figure 6). When the trocars are inserted deeper than expected, injury of the suprahyoid muscles or bleeding may occur. When the trocars are inserted more superficially then expected, there is potential danger of skin injury. Especially, right upon the hyoid bone, there is a wrinkle of the skin, which is the most dangerous place for skin injury during the insertion of the trocars.
The anatomy of anterior neck
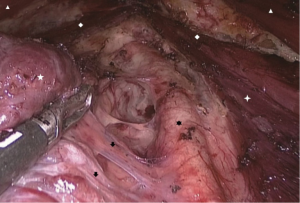
In the neck, the right level of the working space is also in the superficial level of deep cervical fascia beneath the platysma. The working space is upon the superficial fascia of strap muscles and sternocleidomastoids, between the external boundary of the sternal heads of bilateral sternocleidomastoid. It is beyond the sternal jugular notch and bilateral clavicular heads. Once the working space is accomplished, all these landmarks can be found (Figure 7).
In TOETVA, a visible dissection rod is used for blunt dissection from the 1cm incision to suprasternal fossa after injection of the expansion fluid. The visible dissection rod is then moved back to the superior border of thyroid cartilage, and moved in the direction of the lateral boundary of sternal heads both left and right side. Energetic equipment is applied for enlargement of the working space. An ideal working space requires for adequate separation. The internal sternocleidomastoid muscle should be exposed before lobectomy and dissection of central compartment.
For the working space, the superior bound is the upper side of thyroid cartilage and the inferior bound is the sternal jugular notch. The sternal jugular notch located at the superior border of the sternum manubrium, between the clavicular notches, is the most important skeleton landmarks when creating the working space. The sternal jugular notch is critical for searching the sternocleidomastoid and evaluating the depth of working space. Moreover, when dissection of level 3 or 4 lymph nodes is needed, the lateral sternocleidomastoid muscle should be exposed (11).
The anatomy of thyroid gland
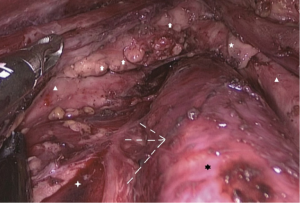
After splitting the linea alba cervicalis completely from the superior boundary of thyroid cartilage to the sternal jugular notch, the isthmus of thyroid gland is exposed. The whole thyroid gland is located posterior to the strap muscles and its isthmus is fixed on the tracheal from the second to the fourth rings of the trachea.
For this part, the skeleton landmarks include the trachea, the thyroid cartilage, the cricoid cartilage and the sternal jugular notch. The trachea is the most important landmark and is the navigator for localization of the thyroid gland and other anatomical structures. Therefore, finding the trachea is the first step in transoral thyroidectomy. The thyroid cartilage is a cartilage that sits in front of the larynx and above the thyroid gland. It is the origin of the sternothyroid muscle, the upper boundary for splitting the linea alba cervicalis and the very upper boundary of the transoral working space. The thyroid cartilage can be exposed by adequately turning the laproscopy vertically. The cricoid cartilage is located below the thyroid cartilage and is the skeleton landmark for dissecting the Delphian lymph node (DLN). The cricothyroid muscle which is located between the thyroid cartilage and the cricoid cartilage, is an important landmark for localization of the cricothyroid space and the thyroid superior pole.
For better exposure of the thyroid upper pole, the superior part of the sternothyroid can be partly cut off closely against the internal boundary connecting to the thyroid cartilage. By traction of the strap muscle upper outwards, the superior thyroid vessels can be well exposed and divided closely against the thyroid upper pole after the pretracheal fascia is exposed (Figure 8).
The thyroid middle vein is usually identified and divided, and cut off closely to the thyroid capsule (Figure 9). Next, the common carotid artery can usually be exposed. The right common carotid originates from the brachiocephalic trunk, while the left originates from the aortic arch. Both arteries split into the external and internal carotid arteries at the upper border of the thyroid cartilage. The inferior thyroid artery runs across the recurrent laryngeal nerves (RLN) near the thyroid lower pole. Therefore, before division of the inferior thyroid vessels, the RLN should be exposed and well protected. The procedure of inferior thyroid vessels is almost always the last part of transoral thyroidectomy. Once the inferior thyroid vessels are cut off, the thyroid lobe is completely excised.
The anatomy of nerves, parathyroid glands and lymph system
Just like open thyroidectomy, in TOETVA, all the surgical procedures also should be performed closely against the true capsule to protect the RLN and the blood supply of parathyroid nodule.
The RLN and the superior laryngeal nerve (SLN), both derived from the vagus nerves, are the most important nerves in thyroidectomy (Figures 10,11). Although the direction in which the RLNs run can be diverse, the entrance of RLN external branch to larynx at the cricothyroid space is relatively fixed and can be easily found under transoral perception. Therefore, the cricothyroid space is important in identification of RLN and is a critical landmark for novices during TOETVA (12). The SLN travels along with the internal carotid artery and divides into two branches at the hyoid bone level. In transoral thyroidectomy, the SLN is hard to expose because of perception, but the SLN should be protected when manipulating the thyroid upper pole.
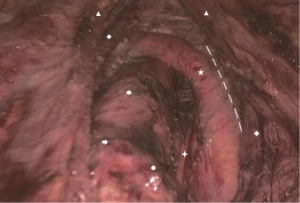
The superior parathyroid glands are developed from the fourth pharyngeal pouch, along with part of the thyroid gland and its location is relatively constant at the dorsal aspect of the upper thyroid lobes at the level of the inferior border of the cricoid cartilage. The inferior parathyroid glands are developed from the third pharyngeal pouches with the thymus and its location is more variable (Figure 11). The blood supply of parathyroid glands originates from the superior and inferior thyroid arteries. In transoral thyroid surgery, the superior parathyroid glands and their blood supply should be kept in situ if possible. To protect the blood supply of the parathyroid glands, surgical manipulation should be performed closely to the true capsule of the thyroid gland and the division of vessels should be performed at the level of the third branch of the thyroid vessels. Moreover, it is important to preserve the thymus during central neck dissection since the latest study indicates preservation of the layer of thymus-blood vessel-inferior parathyroid gland is important for preserving the inferior parathyroid gland in situ (13).
The cervical lymph nodes are classified into seven level. The central compartment (level VI) is between the two carotid sheathes, bound by cricoid cartilage superiorly and sternal notch inferiorly. Comparing to SET via anterior chest access, transoral thyroidectomy has advantage in dissection of the lower part of central compartment (especially lymph nodes behind sternum or clavicle) including level VII lymph nodes.
Conclusions
Transoral thyroidectomy is minimal invasive, safe and cosmetic effective. Transoral thyroidectomy has advantage in manipulation of the lower part of the thyroid gland and the central compartment. Familiarity with the anatomy and landmarks will aid surgeons when dealing with important structures.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Anuwong Angoon, Hoon Yub Kim, Ralph P. Tufano and Gianlorenzo Dionigi) for the series “Transoral Thyroidectomy” published in Annals of Thyroid. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aot.2017.11.03). The series “Transoral Thyroidectomy” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the manuscript and ensure that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ohgami M, Ishii S, Arisawa Y, et al. Scarless endoscopic thyroidectomy: breast approach for better cosmesis. Surg Laparosc Endosc Percutan Tech 2000;10:1-4. [Crossref] [PubMed]
- Ikeda Y, Takami H, Sasaki Y, et al. Endoscopic neck surgery by the axillary approach. J Am Coll Surg 2000;191:336-40. [Crossref] [PubMed]
- Witzel K, von Rahden BH, Kaminski C, et al. Transoral access for endoscopic thyroid resection. Surg Endosc 2008;22:1871-5. [Crossref] [PubMed]
- Nakajo A, Arima H, Hirata M, et al. Trans-Oral Video-Assisted Neck Surgery (TOVANS). A new transoral technique of endoscopic thyroidectomy with gasless premandible approach. Surg Endosc 2013;27:1105-10. [Crossref] [PubMed]
- Wang C, Zhai H, Liu W, et al. Thyroidectomy: a novel endoscopic oral vestibular approach. Surgery 2014;155:33-8. [Crossref] [PubMed]
- Wilhelm T, Harlaar J, Kerver A, et al. Transoral endoscopic thyroidectomy. Part 1: rationale and anatomical studies. Chirurg 2010;81:50-5. [Crossref] [PubMed]
- Wilhelm T, Benhidjeb T. Transoral endoscopic neck surgery: feasibility and safety in a porcine model based on the example of thymectomy. Surg Endosc 2011;25:1741-6. [Crossref] [PubMed]
- Cai C, Huang Y, Zhang T, et al. Anatomical study of surgical approaches for minimally invasive transoral thyroidectomy: eMIT and TOPP. Minim Invasive Ther Allied Technol 2015;24:340-4. [Crossref] [PubMed]
- Park JO, Kim CS, Song JN, et al. Transoral endoscopic thyroidectomy via the tri-vestibular routes: results of a preclinical cadaver feasibility study. Eur Arch Otorhinolaryngol 2014;271:3269-75. [Crossref] [PubMed]
- Wang MQ, Hu KQ. Color Atlas of Practical Oral Anatomy. Xi’an: World Book Publishing Xi’an Co., 2012.
- Yan H, Wang Y, Wang P, et al. "Scarless" (in the neck) endoscopic thyroidectomy (SET) with ipsilateral levels II, III, and IV dissection via breast approach for papillary thyroid carcinoma: a preliminary report. Surg Endosc 2015;29:2158-63. [Crossref] [PubMed]
- Wang Y, Yu X, Wang P, et al. Implementation of Intraoperative Neuromonitoring for Transoral Endoscopic Thyroid Surgery: A Preliminary Report. J Laparoendosc Adv Surg Tech A 2016;26:965-971. [Crossref] [PubMed]
- Wang JB, Wu K, Shi LH, et al. In situ preservation of the inferior parathyroid gland during central neck dissection for papillary thyroid carcinoma. Br J Surg 2017;104:1514-22. [Crossref] [PubMed]
Cite this article as: Zhang M, Xie Q, Wang Y, Wang P. Surgical anatomy for transoral endoscopic thyroid surgery through vestibular approach (TOETVA). Ann Thyroid 2017;2:15.


